Page Contents
OVERVIEW
How could someone order a full chest pain workup when it really is not indicated? Chest pain is one of those chief complaints that really gets medical professionals very excited! There are many can’t miss diagnoses for chest pain that are serious and life threatening, so very often the threshold for ordering studies for a patient with chest pain, is quite low. While this increases the chance that patients with atypical presentations may be diagnosed with life threatening conditions, sometimes the bar for ordering tests for what we classify as “chest pain” might very well be too low.
The case below explains a more clear cut instance in which a chest pain workup really was not necessary (but was conducted twice) in a patient with a very unique case of chest pain.
WHAT HAPPENED?
The patient in question is a 82 year old woman with COPD, GERD, hypertension, and hyperlipidemia who gets admitted to the medical floor with severe chest pain. She has a complicated medical history however it is important to highlight a few important points.
2 weeks ago this patient was worked up for chest pain in the ED. The following tests were ordered (and here are their results):
- EKG: patient has normal sinus rhythm with no abnormalities
- Troponin: within reference range
- Chest X-ray: no remarkable findings
- D-dimer: elevated (~700 ng/mL). This raised concerns for a pulmonary embolism.
- CT-angiography: no abnormal findings, no signs of a pulmonary embolism.
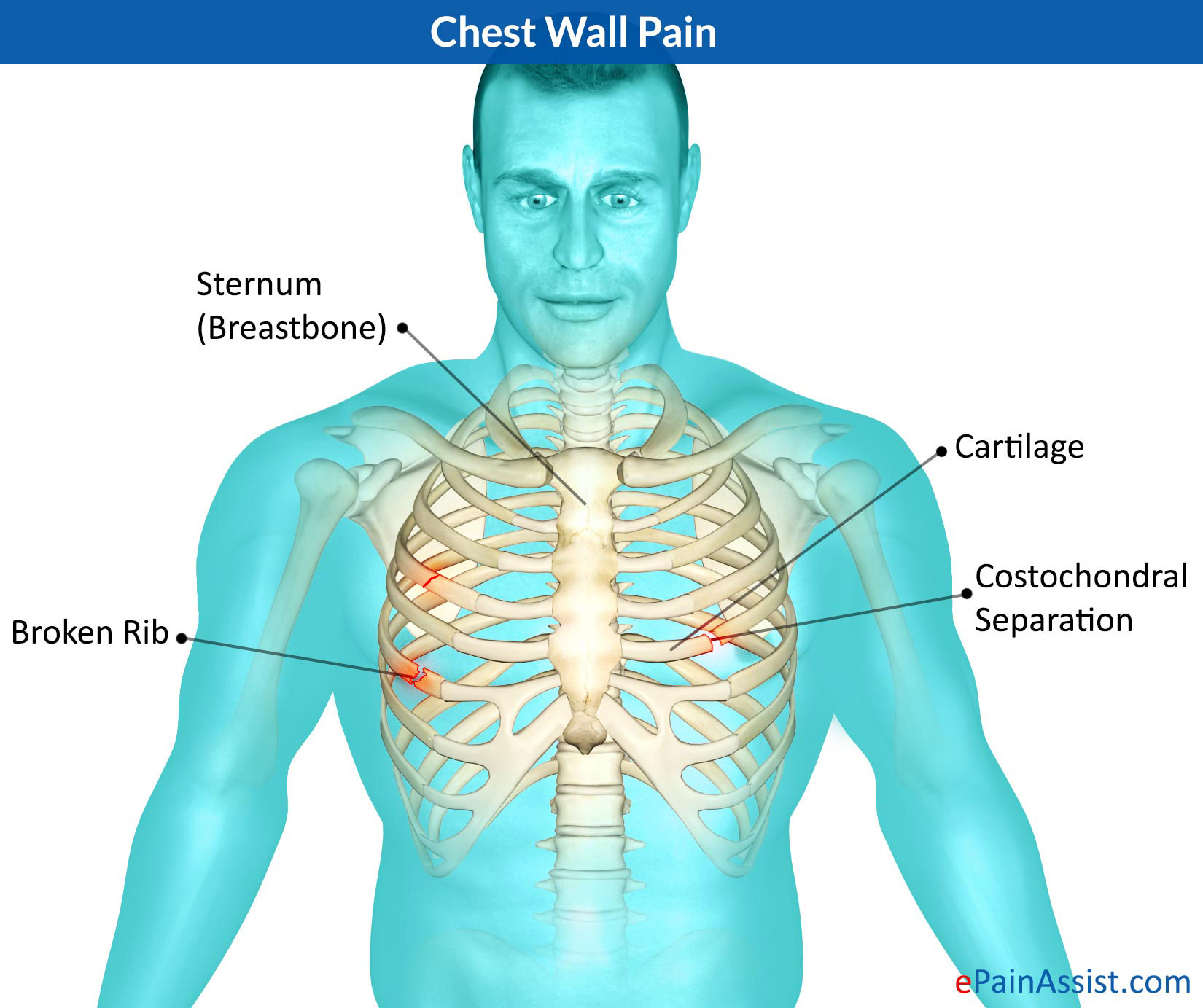
In the end of the ER workup, the patient was diagnosed with “chest wall pain” and sent home with a prescription for Motrin (Ibuprofen).
Coming back to the patient’s current admission the patient again presents with the same chest pain and has the following workup repeated in the ER (before being admitted to the medicine floor).
- EKG: patient has normal sinus rhythm with no abnormalities
- Troponin: within reference range
- Chest X-ray: no remarkable findings
At this point, with no answers upon evaluation in the ER, the patient is admitted to the floor for further workup. Upon evaluation on the medicine floor a few very important points come to light.
- The patient’s vitals are all stable.
- This patient’s chest pain can be localized to the sternum, and it radiates to both breasts slightly.
- The patient’s chest pain is positional (moving around in bed will cause her pain to worsen)
- This patient has been having this identical chest pain for 2 weeks (i.e. this chest pain is identical to that worked up in her first ER visit, and it has remained unchanged for the past 2 weeks).
- This patient experiences severe pain when her sternum/either side of her upper chest is touched. Even a slight touch with gentle pressure causes the patient to experience chest pain.
- There are no skin findings on the chest that explain the patient’s presentation.
- The rest of the patient’s exam is completely unremarkable.
- The patients CRP was not elevated.
With this information, the team digs deeper into the patient’s medical record. They find that during the past ER workup, one note comments that a friction rub was heard when auscultating the heart. Even though no friction rub is heard on the current exam, the team decides to order an echocardiogram the following day to rule out pericarditis/pericardial effusion. In the meantime the patient is given Tramadol and Acetaminophen for pain before going to bed.
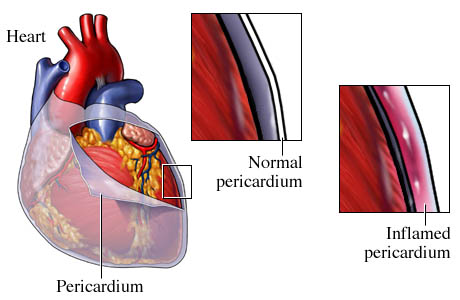
The next morning when the patient is examined she explains that her pain is completely gone. What was once a 10/10 on the pain scale is now a 0/10. She thanks the medical team for all that they have done, and explains this is the first time that she has been cared for well as a patient. She wishes to go home and tells the team that she is looking forward to baking brownies and cooking. She is excited to leave the hospital as soon as possible, however the team convinces her to stay for her scheduled echocardiogram so they can rule out pericarditis.
The echocardiogram is performed and no pericarditis is found. The patient is discharged to her home without the need for any prescribed pain medication. It was decided that very likely this patient had a musculoskeletal or psychological cause of her pain (given the clinical workup above).
AT WHAT POINT DID THE FOREST BECOME LOST IN THE TREES?
It seems that this rich and complex case has many instances in which the “bigger picture” was lost:
The patient exam: this level of tenderness across the sternum (and such sharp pain with light touch over the area of the chest) is a completely atypical type of chest pain that can really not be explained by any of the can’t miss diagnoses. While there are always exceptions to presentations, we must think very strongly about the utility of the initial tests ordered (EKG, Troponin, Chest X-ray, D-dimer, CT-angiography) in helping to characterize this type of chest pain. What disease process can be diagnosed by these tests that would cause sternal pain with light touch?
The repeat ER workup: this patient came to the ER a second time with the SAME COMPLAINT. At this time point, the question arises why repeat the tests ordered on the initial admission, if this is for the same persistent/chronic issue (that was not informed by these tests on the initial evaluation?). While the patient history can sometimes be unreliable, the patient made it very clear that this was the exact same pain she was experiencing on her previous workup, and it had remain unchanged for the past 2 weeks.
The hospital admission: looking at the patient clinical course, after the second admission one can ask the question as to why exactly the patient was admitted to the hospital after the second ER workup did not find any cause of her chest pain? Was it to perform the echocardiogram? We can discuss this below.
Ordering the echocardiogram: while it is true that 2 weeks ago it was documented that the patient was thought to have a friction rub, is this really all it takes to justify ordering an echocardiogram? The patient has no signs of pericarditis/pericardial effusion on the exam, her vitals are stable, her chest pain can to be explained by these disease processes, and what’s more, her CRP (often elevated in inflammatory processes like pericarditis/pericardial effusion) is not elevated. Was this test ordered to legitimately rule out likely diagnosis? Or to just “do something?”.
Performing the echocardiogram: between when the echocardiogram was ordered, and when it was performed, the patient had a complete resolution of symptoms. One has to ask themselves….if the issue that warranted ordering the echocardiogram has resolved…does it still make sense to perform this study? Especially in light of the patient’s presentation and low likelihood for having pericarditis/pericardial effusion?
WHY SHOULD WE NOT THINK ITS COMPLETELY “CRAZY” THAT THIS HAPPENED?
As stated before, chest pain really causes a very reflexive response in medical providers with regards to ordering studies for a workup. Many causes of chest pain can sometimes present in an atypical manner, so ordering an EKG, Troponin, and Chest X-ray can help evaluate for many of the classic causes of chest pain (without too much effort).

Whats more, this patient is older, and missing a serious illness in someone like this could be potentially fatal. It is important to realize that often erring on the side of caution can save lives, and that as providers we must be thorough in our workup of patients.
WHO CARES? WHAT WAS THE HARM IN WHAT HAPPENED?
This was an incredibly time intensive, expensive, and extensive workup that ultimately culminated in sending the patient home without effectively having done ANYTHING.
WHAT IS THE TEACHING POINT HERE? HOW DO WE AVOID THIS IN THE FUTURE?
There are a few important teaching points to take away from this case:
- Characterize the chief complaint well: chest pain can manifest differently. Chest pain that is tender to light touch (over the sternum) is not the same is chest pain that radiates to the arm/jaw. The nature of the pain gives clues as to what is going on!
- Don’t undersell the physical exam: many components of the physical exam can often be crude and unhelpful at times. That being said, when it comes to chest pain, visualizing and palpating the chest can be very informative! Evaluating for dermatological and/or musculoskeletal causes of chest pain can help dramatically change the workup.
- Don’t order tests “just because”: in the case of this patient it seems many of the ordered exams could have been avoided. Going to the most clear example of this, the echocardiogram simply had no justification for being ordered in the beginning. Whats more, after the resolution of the patient’s symptoms it made even less sense to perform this study! The team was never truly considering pericarditis/pericardial effusion.
Page Updated: 09.27.2016