OVERVIEW
While also components of the neurological exam, mental status and cranial nerve exams have been covered in separate documents (mainly for the sake of simplicity). This page deals exclusively with the other components of the neurological exam that include:
- Muscle strength
- Reflexes
- Sensation
- Muscle tone
- Supplemental Exams
MUSCLE STRENGTH
The order of neurological exam components can vary depending on the clinical scenario, however generally speaking (and under screening circumstances) this portion of the exam can begin immediately after examining the cranial nerves of the patient. When assessing strength keep a few things in mind:
- Testing each side independently is important
- Comparing opposite sides of the body is useful in order contextualize the relative strength of the patient in each side
- Isolating the muscles that you are testing is critical (place hands on opposite sides of the joint involved in the test)
Upper extremities: test strength in deltoids, biceps, triceps, wrist extensors, finger extensors, dorsal interosseous muscles.
Lower extremities: test strength in psoas, hamstrings, quadriceps, dorsiflexors.
Grading scale:
0- No muscular contractoin detected
1- Barely detectable contraction
2- Active movement of the body part, but not against gravity
3- Active movement against gravity possible
4- Active movement against gravity and some resistance
5 – Active movement against full resistance without any fatigue
REFLEXES
Below are the locations where reflexes can be tested for this portion of the exam:
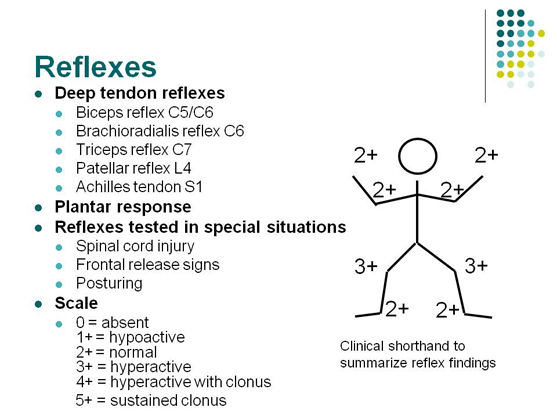
Clonus: can be checked in the manner shown in this video.
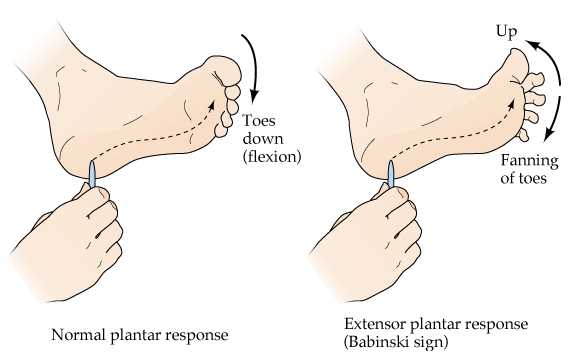
Plantar reflex: also called the Babinksi sign. This can be assessed by scraping the bottom of the foot with an object. An upping toe is a sign of an upper motor neuron issue.
SENSATION
Sensation can be tested most anywhere on the body (the exact locations will depend on the specific clinical presentation you encounter). One of the most important things to keep in mind is that there are 2 sensory pathways (both of which can be tested with a broken sterile cotton swab).
- Pain/temperature sensory pathway: the broken side of a cotton swab can serve to test the pain component (pinprick).
- Light touch/proprioception/vibration: the cotton end of the swab can assess for intact light touch sensation.

MUSCLE TONE
Muscle tone refers to the small level of contraction that muscles have when relaxed. Normal muscle tone will provide slight resistance to movmeent. When checking for muscle tone have the patient relax and allow you to passively move their limbs. Certain findings can be useful for making diagnosis in patients:
- Spasticity: this refers to velocity dependent catching (high levels of tone experienced only when moving the limb quickly) and is suggestive of upper motor neuron issues.
- Lead pipe rigidity: this refers to increased tone that is not velocity dependent, and is always present (i.e. trying to bend a lead pipe). This is suggestive of a condition like Parkinson’s.
SUPPLEMENTAL EXAMS
Below are some special exams that can be used to further evaluate patients.
Asterixis: have the patient hold out their arms and flex their hands backward (as if they are stopping traffic). Push back on the patients hands. If a sporadic tremor is seen, (such as this one) that can be characterized by “hand flapping” this is referred to as asterixis. This can be a sign of hepatic encephalopathy, alcohol withdrawal, and is associated with cirrhosis of the liver/acute liver failure).

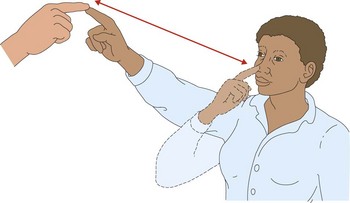
Cerebellar function: the cerebellum is responsible for coordinating movements. Much like a police officer might do in a suspected drunk driver, we can assess cerebellar function clinically.One example of this is the nose to finger test, which is exactly as it sounds: the patient alternates between touching their nose to your finger.
Romberg Test: This is a test of proprioception sensory pathways NOT CEREBELLAR FUNCTION. The patient is asked to stand erect with both feet together, and then the patient is asked to stand with their eyes closed for ~30 sec. A positive Romberg test is if the patient sways, loses balance, or becomes MORE unsteady after closing their eyes (if unsteady even with eyes open this is more suggestive of cerebellar dysfunction. Possible causes can include any that affect the dorsal column of the spine, or the peripheral sensory pathways (vitamin B12 deficiency, CIPD, Friedreich ataxia, and tabes dorsalis.
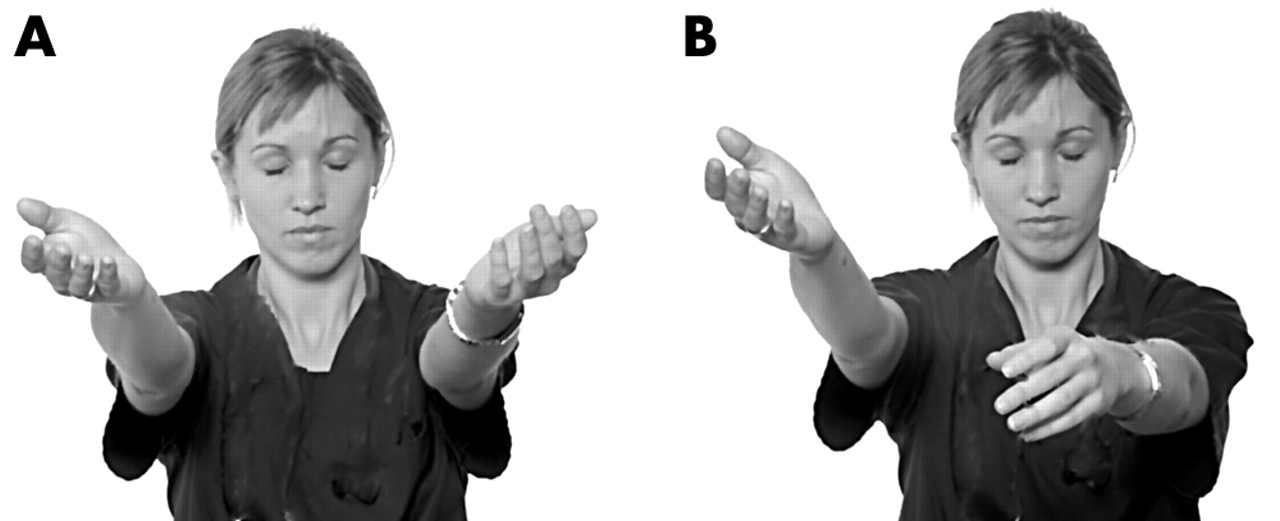
Pronator Drift: This tests for upper motor neuron weakness. The patient is asked to extend their arms straight in front of them, with their palms to the sky. The patient is then asked to close their eyes, and any drifting of the palms to the pronated position is noted (positive sign for pronator drift).
Gait: observing a patient’s gait can be informative with regards to the underlying cause of possible neural dysfunction. For example: individuals with cerebellar dysfunction will have a wide based gait for stability. Have a patient walk away from you, turn, and then walk back towards you (paying special attention to foot placement, walking speed, nature of turn, etc.)
Heel/Toe walking (spinal nerves): having a patient walk both on their heels and toes after examining normal gait can be useful in assessing the possibility of a disk herniation in L5-S1 (most common location for a herniation).
- Toe walk: this type of walking tests the strength in the gastrocnemius (calfs) which is controlled by the S1 nerve root.
- Heel walk: ankle and toe dorsiflexor muscles are used for this, which is controlled by L5 (and some L4) nerve roots.
Page Updated: 01.23.2016