Page Contents
- 1 WHAT IS IT?
- 2 WHY IS IT A PROBLEM?
- 3 WHAT MAKES US SUSPECT IT?
- 4 CLINICAL WORKUP
- 5 AT WHAT POINT ARE WE COMFORTABLE IN MAKING THE DIAGNOSIS
- 6
- 7 HOW DO WE TREAT IT?
- 8 HOW WELL DO THE PATIENTS DO?
- 9 WAS THERE A WAY TO PREVENT IT?
- 10 WHAT ELSE ARE WE WORRIED ABOUT?
- 11 OTHER HY FACTS?
- 12 ARCHIVE OF STANDARDIZED EXAM QUESTIONS
- 13 FURTHER READING
WHAT IS IT?
Preeclampsia is a complication during pregnancy that is characterized by hypertension, proteinurea, and edema after the 20th week of pregnancy.
WHAT CAUSES IT?
It is thought to be caused by abnormal placental spiral arteries (other hypothesis exist as well). This condition can progress to eclampsia if the patient also experiences seizures.
WHY IS IT A PROBLEM?
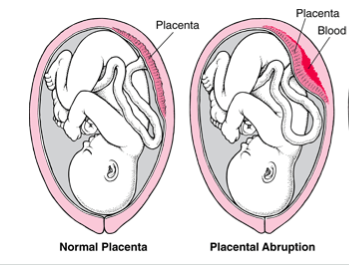
These abnormal spiral placental arteries lead to endothelial dysfunction, vasoconstriction, and ischemia. This can ultimately lead to complications including: placental abruption, coagulopathy, renal failure, uteroplacental insufficiency.
Whats more, patients with preeclampsia may at be at risk for generlaized seizures in this disease setting (eclampsia).
WHAT MAKES US SUSPECT IT?
Risk Factors:
Pre-existing hypertension, diabetes, chronic renal disease, autoimmune disorders
Initial Presentation: This complication will often first arise in patients who are pregnant
- New onset hypertension
- Edema
- Abdominal pain
- Vision changes
Physical Exam:
Vitals:
- Hypertension: systolic blood pressure ≥ 140 mm Hg and/or diastolic blood pressure ≥ 90 mm Hg
Respiratory exam:
- Pulmonary edema: this is a complication of severe preeclampsia and “crackles” amy be heard upon auscultation the lung fields.
Cardiovascular exam:
- Edema: that can affect hands and feet (with associated weight gain)

CLINICAL WORKUP
Urine dipstick: patents with preeclampsia may have 1+ protein on this test. While 1+ protein on this study is diagnostic of proteinuria, due to the high false-positive and false negative rate of this study, it all results should be confirmed with either a urine protein/creatine ratio, or a 24-hour urine collection for total protein.
- Protein/creatinine ratio: proteinuria (diagnostic for preeclampsia) defined as ≥ 0.3
- 24-hour urine collection for protein: a value of > 300 mg is diagnostic for preeclampsia
AT WHAT POINT ARE WE COMFORTABLE IN MAKING THE DIAGNOSIS
Reference:
The materials below are in referees to the 2013 ACOG criteria (source).
General diagnosis:
Hypertension (blood pressure ≥ 140/90 mm Hg) and proteinuria (> 300 mg/24 hours) after 20 weeks gestation.
If no proteinuria is present:
If the patient does not have any proteinuria, then the diagnosis of preeclampsia requires one of these other findings. These all are thought to demonstrate end-organ damage.
- Thrombocytopenia (< 100,000 platelets/mcL)
- Impaired liver function (increased serum liver transaminases to 2x normal concentration)
- Severe, persistent, right upper quadrant pain that is not explained by an alternative diagnosis, and is refractory to medicine
- Renal insufficiency that is progressive (increased serum creatinine > 1.1 mg/dL or doubling of serum creatinine in patient without other renal disease)
- Pulmonary edema
- New-onset of cerebral or visual disturbances (this can include headache)
Severe preeclampsia:
A noteworthy distinction in this diagnostic realm is between preeclampsia and severe preeclampsia (because severe preeclampsia may need to be managed more aggressively). The diagnosis of severe preeclampsia is given if the any of the following conditions are met (essentially any signs of possible end-organ damage gain a patient this diagnosis of severe preeclampsia).
- More severe hypertension defined as ≥ 160 mm Hg or diastolic blood pressure ≥ 110 mm Hg (taken on 2 occasions at least 4 hours apart during bed rest)
- Thrombocytopenia (< 100,000 platelets/mcL)
- Impaired liver function (increased serum liver transaminases to 2x normal concentration)
- Severe, persistent, right upper quadrant pain that is not explained by an alternative diagnosis, and is refractory to medicine
- Pulmonary edema
- New-onset of cerebral or visual disturbances (this can include headache)
HOW DO WE TREAT IT?
Delivery: this will effectively cure the condition, however should only be done at a gestational age ≥37 weeks
Antihypertensives: such as Labetalol (Selective α1- and nonselective β-adrenergic blocking agent)
IV magnesium sulfate: is used to prevent seizures/eclampsia
HOW WELL DO THE PATIENTS DO?
Once patients deliver their child/children they no longer will suffer form this condition (placental arteries are no longer present). The hypertension should usually resolve within 6 weeks.
WAS THERE A WAY TO PREVENT IT?
Women who are at higher risk for developing preeclampsia might benefit from taking aspirin source
WHAT ELSE ARE WE WORRIED ABOUT?
HELLP syndrome: this is a manifestation of severe preeclampsia. The acronym comes from: Hemolysis, Elevated Liver enzymes, and Low Platelets. Schistocytes can be seen on smear. This can lead to sub capsular hematoma (which can then cause severe hypertension by rupturing). The treatment of this is immediate delivery.
Pulmonary edema: this can be a life threatening complication of severe preeclampsia.
Placental abruption: either partial or complete separation of the placenta from the uterine wall before delivery (can be caused by preeclampsia).
OTHER HY FACTS?
Preeclampsia + seizures = eclampsia
ARCHIVE OF STANDARDIZED EXAM QUESTIONS
This archive compiles standardized exam questions that relate to this topic.
FURTHER READING
Page Updated: 01.26.2016