Page Contents
- 1 WHAT IS IT?
- 2 WHAT CAUSES IT?
- 3 WHY IS IT A PROBLEM?
- 4 WHAT MAKES US SUSPECT IT?
- 5 CLINICAL WORKUP
- 6 AT WHAT POINT ARE WE COMFORTABLE MAKING THE DIAGNOSIS?
- 7 WHAT ELSE ARE WE WORRIED ABOUT?
- 8 HOW DO WE TREAT IT?
- 9 HOW WELL DO THE PATIENTS DO?
- 10 WAS THERE A WAY TO PREVENT IT?
- 11 OTHER FACTS?
- 12 ARCHIVE OF STANDARDIZED EXAM QUESTIONS
- 13 FURTHER READING
WHAT IS IT?
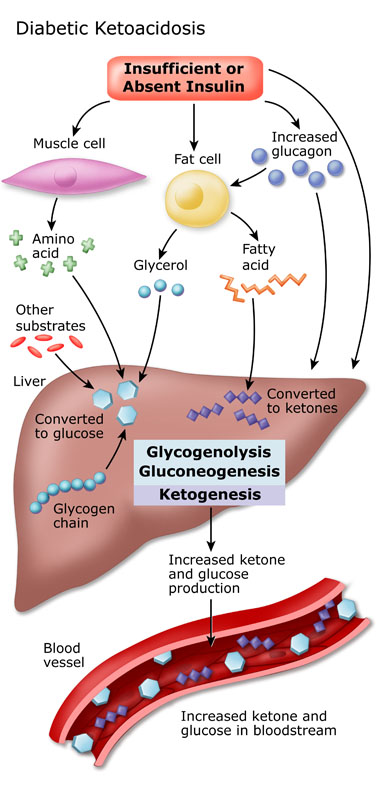
Diabetic ketoacidosis refers to a physiological state in a diabetic patient, where even in the presence of high serum concentrations of glucose, there is extreme ketogenesis (i.e. fat metabolism) that will cause lowered blood pH. This lowered blood pH (acidosis) is a direct result of the produced ketones that are acidic in chemical nature.
It is characterized by 3 major components:
- Hyperglycemia: high serum glucose concentrations
- Acidemia: low serum pH levels
- Presence of ketones: found in the serum and/or in the urine
WHAT CAUSES IT?
Fundamentally this condition is caused by a mismatch between the insulin demand and activity within the body of a patient. When the insulin demands are much higher then the functional activity of insulin, cells throughout the body are glucose starved, and must resort to fat metabolism to maintain the function of important tissues (such as the brain). The bi-product of this fat metabolism is the production of acidic ketone bodies (which are utilized for ATP production in peripheral tissues/the brain).
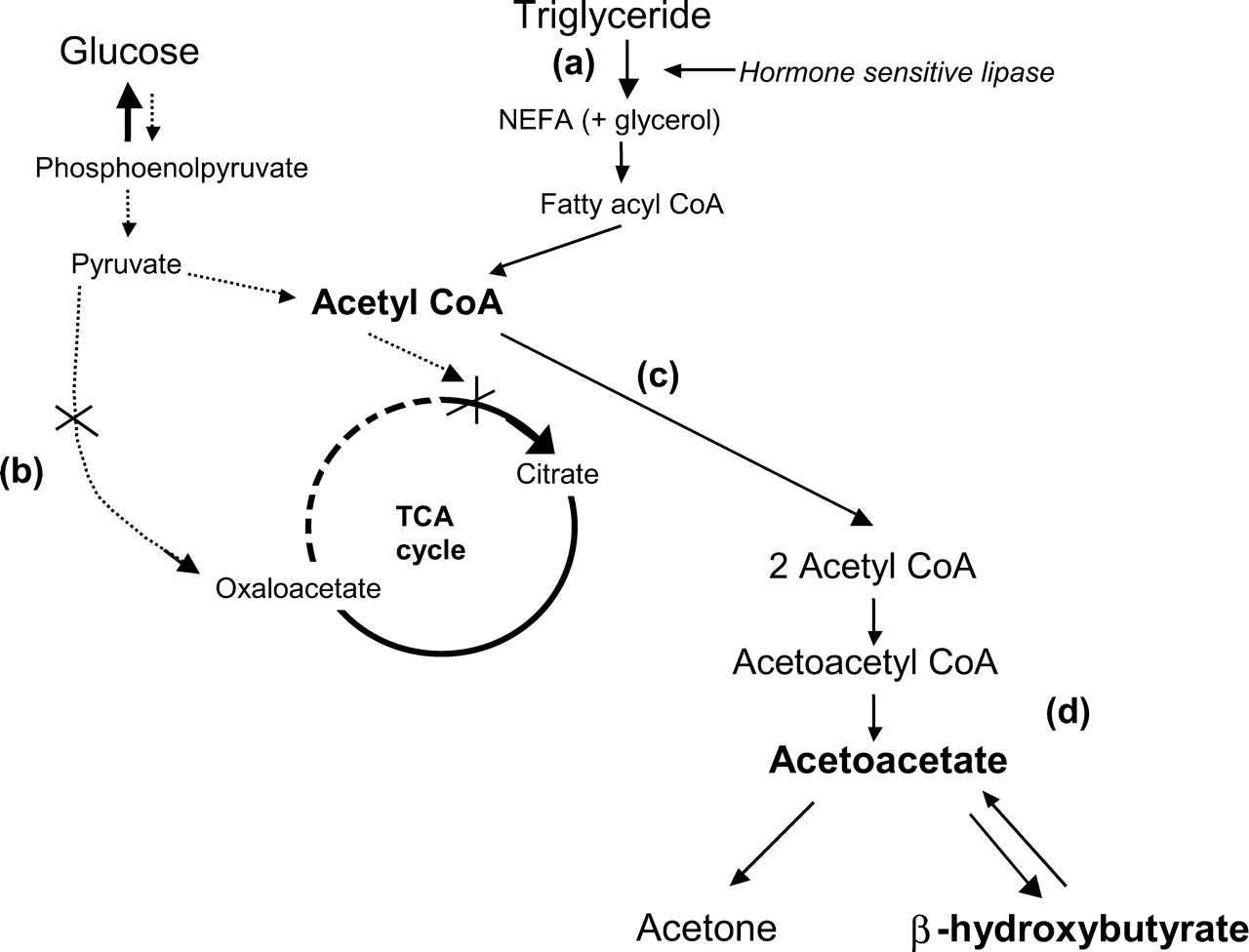
Realistically this condition will often occur in the setting of poorly controlled diabetes (type 1 diabetes is more common given that type 2 diabetics often have some basal insulin levels that offset this process) in which there is some baseline ketogenic state. This typically will sensitize patients to develop DKA, but it is not sufficient to cause the condition on its own. In this setting additional stressors to the body (such as infections) are the precipitants of DKA due to their ability to induce glucagon secretion through the epinephrine pathway (epinephrine will stimulate glucagon recreation). This increase of glucagon will not only further activate fat breakdown, but will also increase blood glucose levels (by moving intracellular glucose into the serum of the patient).
Common precipitants of DKA can include:
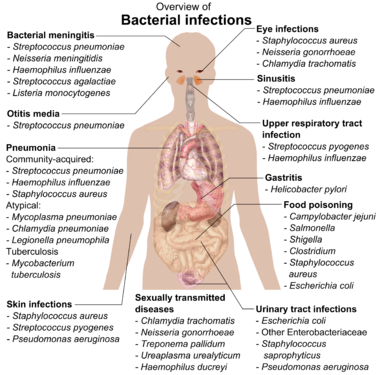
- Infection that can be most anywhere in the body
- Acute pancreatitis that can be secondary to gallstones, alcohol usage, drug reactions, etc.
- Myocardial infarction
WHY IS IT A PROBLEM?
The combination of severe acidosis and the lack of glucose metabolism really does not bode well for the health of the patient. The human body operates within a certain pH range, and lowering serum pH (by any mechanism) can lead to damage of various structures, tissues, cells, proteins throughout the body.
Furthermore given that the underlying precipitant of DKA can also be an infection, this type of infection itself can be problematic (and needs to be addressed in addition to treating the DKA).
The consequence of hyperglycemia will also be increased osmotic diuresis and can cause severe dehydration.
WHAT MAKES US SUSPECT IT?
Risk Factors:
Type 1 diabetes (can be poorly controlled diabetes) PLUS current stressor (UTI, pneumonia, MI)
Initial Presentation:
Chief Complaints:
- Mental status changes: might be noticed by the patient or those around them
- Nausea/vomiting
- Abdominal pain
- Generalized weakness
History Of Present Illness:
Onset: the emergence of symptoms is generally acute (~1-2 days).
Insulin usage may be intermittent, recently stopped, or patients may not be using insulin at all.
Associated symptoms can include polyuria/polydipsia (due to hyperglycemia)
Physical Exam: it is important to utilize the physical exam in such patients to try and localize if there is any source of infection that requires targeted treatment.
Vital signs may show various findings depending on the volume status, extent of academia, and presence of infection in the presenting patient.
- Vitals consistent with dehydration may be observed (hypotension, reflex tachycardia)
- Fingerstick glucose verified hyperglycemia: a finger-stick may be acquired in some care settings with other vital signs. This will show hyperglycemia in patients with
HEENT exam can show:
- Signs of dehydration: dry mucous membranes (signs of dehydration).
- Fruity breath odor: this is caused by the presence of acetone (a ketone) in the blood.
Respiratory exam might reveal:
- Kussmaul respirations are “classically” seen in DKA.
- Signs of pulmonary infection: crackles/auditory findings on auscultation may be present in some patients.
Abdominal exam could be notable for:
- Abdominal pain that might suggest pancreatitis/or other abdominal pathologies.
- Generalized/nonspecific abdominal pain may also be observed.
CLINICAL WORKUP
Clinical Goal Of Diagnosing DKA: the following studies are used clinically to help diagnose if a patient is actually experiencing DKA.
Fingerstick glucose: if it has not been collected already (with the vitals) then patients should quickly receive a fingerstick glucose test to confirm for the presence of hyperglycemia.

Basic metabolic profile (BMP): this lab study will help evaluate a few things. We would expect to see the following on a BMP from a patient with DKA.
- Hyperglycemia: the results of this test should confirm a previous fingerstick
- Lowered serum bicarbonate level: often DKA patients will have a level below < 18 mEq/L
- Elevated anion gap (calculator here): patients typically will have an anion gap above 10 (caused by the ketone acids)
- Pseudohyponatremia: glucose osmoles will increase presence of water in blood/serum, diluting the sodium present so patients may also seem hyponatremia.
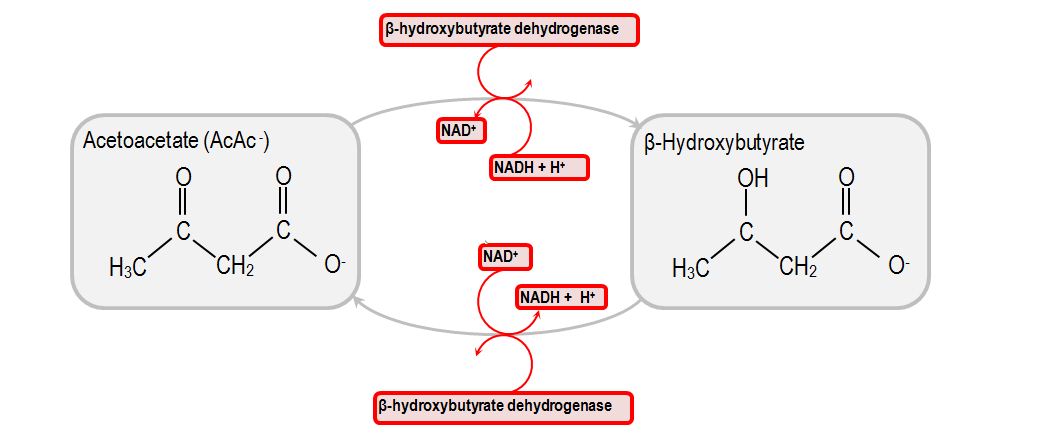
Ketones in the serum: specific blood testing will show the presence of β-hydroxybutyrate (higher levels) and acetoacetate (lower levels) in the serum of patients with DKA
Urinalysis can reveal:
- Ketones: typically urine studies do not detect β-hydroxybutyrate, but will be positive for ketones.
- Glucose: given the hyperglycemia observed, urine glucose levels will be expected to be elevated.
Serum blood gasses can be collected (ideally using arterial blood) to assess for academia:
- Blood pH levels below 7.3 are generally seen in patients with DKA.

Clinical Goal Of Searching For Precipitant: the following studies are more geared towards trying to understand why the presenting patient developed DKA to begin with.
Complete blood count (CBC): this study will often be ordered in the emergency room and can provide some useful information.
- Elevated white blood count can be observed in patients with an infection (but is of course a non-specific finding).
EKG + serum troponin values: in the right patient population, with the right suspicions for myocardial infarction, these studies can help diagnose an MI.
Serum lipase and amylase: these serum values can be assessed in patients with abdominal pain suspicious for pancreatitis and can help be used to confirm the diagnosis.
Urinalysis (also discussed above) can be used to search for signs of infection:
- Leukocyte esterase positive
- Nitrates positive
- Presence of WBCs
- Cultured pathogen from urine
AT WHAT POINT ARE WE COMFORTABLE MAKING THE DIAGNOSIS?
DKA is formally characterized by a number of criteria (read more here) however really there are a few major points that are essentially required for diagnosing this condition (and are core to even the name DKA!).
- Hyperglycemia (> 250 mg/dL): in its absence DKA really can not be the diagnosis.
- Presence of ketones (either serum or urine): in the absence of actual ketones diagnosing DKA is essentially impossible as the patient is not in a ketogenic state!
- Metabolic Acidosis (blood pH <7.3 with anion gap > 10): given the nature of this condition, some level of true acidosis should be observed. Given it is caused by ketones, the anion gap should be elevated to some extent.
**KEEP IN MIND THAT THE ABOVE VALUES ARE SUGGESTED CUTOFFS** it is important to use one’s clinical judgment and not blindly follow these values. Patients on the cusp of these values may still have DKA and will require treatment
WHAT ELSE ARE WE WORRIED ABOUT?
Treating the underlying precipitants: it will be of course in our best interest to make sure we direct treatment to what has caused this DKA in the first place. Let us not forget 3 major causes of DKA (each which will have their own treatment strategy)
- Infection
- Pancreatitis
- Myocardial infarction
Cerebral edema can occur in patients with DKA (usually children) that greatly increases the mortality rate for the condition.
Noncompliance with insulin dosing patients who do not adhere to their insulin regiment can present with DKA. Make sure to check if the medical regiment is clear with a patient who has DKA. This can be done after the patient is stabilized
HOW DO WE TREAT IT?
*THE OVERALL GOAL OF TREATMENT IS TO STOP THE ACIDOSIS BY HALTING THE KETOGENIC STATE!*

The timing of interventions can get confusing due to their overlapping nature: with this in mind we should review the fundamental elements of therapy and why they are conducted:
- Fluid resuscitation: this is used to rehydrate the patient and restore volume status.
- Insulin treatment: this will be used to reverse the ketogenic state and close the anion gap.
- Potassium replacement: our treatments above will decrease serum potassium levels in 2 major ways. One mechanism will be the movement of potassium into cells upon insulin administration. The other will be renal excretion of potassium as the kidneys filter more urine.
- Electrolyte replacement: other electrolytes other then potassium may also require repletion in certain patients.
- Bicarbonate administration: this is typically only reserved for patients who have a very low pH.
IV fluids are given in a “fluid” (pun intended) manner:
- Initially patents are given 0.9% saline to rehydrate patients.
- Once serum glucose is lowered (250-200 mg/dl) patients should be switched to 5% dextrose with 0.45% sodium chloride to avoid causing hypoglycemia.
Insulin administration typically is given as a continuous drip: this process can begin as the fluids are administered.
Potassium/electrolyte repletion: this can occur with the administration of fluids the initial electrolyte values (and subsequent labs) should inform how much electrolytes should be given.
HOW WELL DO THE PATIENTS DO?
This is a serious condition that can be fatal if not treated correctly and promptly. The mortality rate is 1-5% in DKA (source)
WAS THERE A WAY TO PREVENT IT?
Adherence to insulin regiments can prevent some causes of DKA, however certain triggers for this condition can be more difficult to prevent.
OTHER FACTS?
DKA is common in type 1 diabetes, but uncommon in type 2: this is due to the low levels of insulin that are usually present within type 2 diabetes (which prevent DKA from occurring).

ARCHIVE OF STANDARDIZED EXAM QUESTIONS
This archive compiles standardized exam questions that relate to this topic.
FURTHER READING
Page Updated: 08.02.2016