Page Contents
OVERVIEW
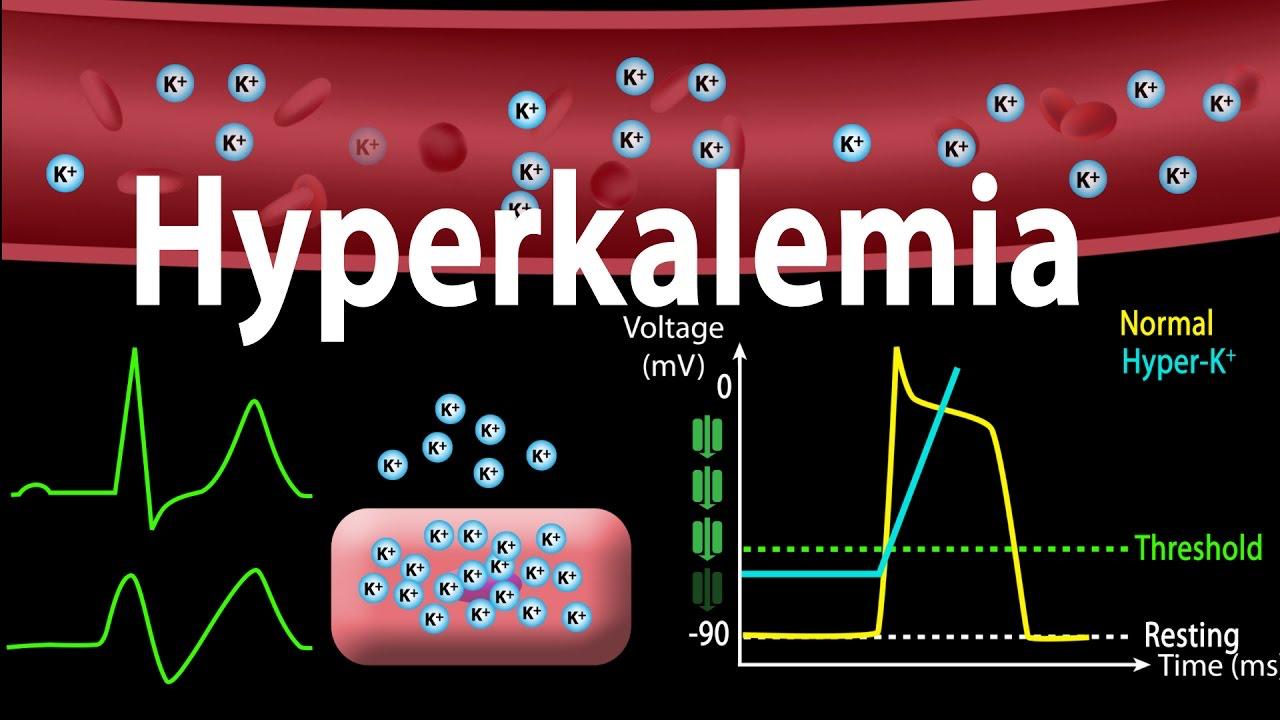
It may be a page from a nurse, a call from the chemistry lab, or you may notice it on the basic metabolic profile (BMP) yourself when reviewing information in the chart. Regardless of how it is detected, hyperkalemia can be a life threatening condition that warrants a clear and thoughtful management strategy. There are many different resources on hyperkalemia that exist (ranging from its differenteial to its management strategies) however this guide is dedicated towards answer the question of what you should do specifically when faced with the patient who has an elevated potassium level.
This page includes tutorial videos in some of its sections (that demonstrates how to perform these features on the UCSF EPIC EMR system). All of these videos can be found in this folder here.
*While the preview feature for these videos may not work on certain mobile browsers, the videos can still be viewed if they are given time to load/the page is refreshed.
STEP 1: BEFORE YOU GET TOO EXCITED, MAKE SURE IT IS REAL HYPERKALEMIA
Initially when faced with any type of situation it is incredibly important to verify that the medical condition you are preparing to treat is in fact what is going on. In the case of hyperkalemia it is critical (before getting too excited) to make sure that the patient actually has hyperkalemia. Here should be the initial though process:
- Check the chart and verify the potassium value: while in many settings a potassium value above 5 mEq/L causes alarm, in reality the upper limit of normal can include 5.5 mEq/L. this does not mean we ignore values below 5.5 mEq/L however this contextualizes the severity of the hyperkalemia.
- Check to see if there is any lab comment about a hemolyzed sample: it is common for labs to be run on hemolyzed blood, which will lead to a falsely elevated potassium in the sample because of the intracellular potassium that is released during hemolysis. This does not mean we ignore any potassium value with hemolyzed blood however it warrants repeat labs to evaluate if it is a true potassium value being reported.
- Evaluate other labs drawn at the same time to see if there are unusual patterns: it is sometimes useful to see if other labs that were drawn at the same time too see if there are many values that are suspiciously outside the ranges of normal limits. One situation that can result in this is if labs are drawn from a line that is administering TPN (all the contents of the TPN may cause falsely elevated lab values that can sometimes be very obvious).
STEP 2: UNIVERSAL ORDERS THAT CAN BE ORDERED ON MOST ALL PATIENTS WITH HYPERKALEMIA
In the context of your above scrutiny, this section will cover orders that can be safely placed on most all patients with hyperkalemia/suspected hyperkalemia. This is not to say that all of these should be ordered every time a patient is thought to have hyperkalemia, however generally speaking, if these were all ordered no harm would be done to the patient and valuable information could be gathered in the majority of hyperkalemia cases. They have been organized by category.
Confirm The Diagnosis:
- Repeat BMP (STAT, fresh blood draw): especially if there is concern for lab error or factors that will cause false elevation of potassium (however typically will always be ordered to confirm the value and/or trend). Make sure to appreciate the creatinine trend to appreciate renal function.
- Fingerstick glucose (POC): while the BMP will reveal the serum glucose level, in some cases a patient may have a high suspicion for an elevated glucose level (such as patients with diabetes) which may be driving their hyperkalemia. The finger-stick will result more quickly then the BMP so sometimes it is appropriate to order both.
Contextualize Renal Function:
- Order updated Ins/Outs to be charted: very likely during the discovery of hyperkalemia not all of the patient’s intake and output data will be updated in the chart. A nursing text order can be placed to ask for this to be done so the patient’s urine output can be contextualized as a proxy of renal function. If strip I/Os are not ordered for the patient make sure to order them!
- Order bladder scan if urine output is low (<30 mls/kg/hour): if the patient is not making appropriate volumes of urine, the differential is broad (and often is pre-renal in origin) however it is useful to quickly see if the bladder is full signifying some type of issue with bladder emptying/obstruction which could be responsible for the elevated potassium.
Stop Iatrogenic Casues Of Hyperkalemia That Will Exacerbate The Issue:
- Stop any potassium repletions/repletions that include potassium (discontinue any active repletion orders/inform nurses to stop current repletions with text order): even if the elevation is mild, there is no reason to worsen it by giving patients more potassium. This includes obviously both PO and IV forms of potassium chloride, however IV potassium phosphate and PO potassium phosphate tablets/packets can also be culprits that should be stopped.
- Switch the patient to a low potassium diet (unless NPO): there is no reason to allow for the patient to eat more potassium unnecessarily if they have a diet.
- Switch IV fluids if they contain potassium (Normal Saline can be used instead, exceptions may exist): while the amounts of potassium in most IV fluids are not large, in certain situations it is prudent to eliminate the delivery of any extra potassium to the patient (especially IV).
- Stop/consider stopping any medications that may worsen hyperkalemia: this will depend entirely on the clinical context however in this moment any other iatrogenic causes of the hyperkalemia should be evaluated and stopped if they are not clinically necessary. Some culprits include (ACE inhibitors, ARBs, Bactrim, digoxin, heparin, NSAIDs)
Evalaute For Signs Of Cardiac Compromise:
- EKG (12 Lead Unit Performed Study, STAT): not every patient will require an EKG, however in most cases it will be ordered to provide comprehensive care. If there is any concern that they patient has true hyperkalemia there is little to no reason to hesitate in ordering an EKG. Signs of cardiac compromise can be evaluated quickly and inform future management.
Protect The Heart:
- Calcium gluconate (1 gram IV, typically can administer 10 mls of a 10% solution as IV push over 2-3 minutes, can be repeated after 5 minutes if necessary): ideally calcium gluconate will be given based upon EKG results (EKG changes will warrant its administration) HOWEVER if there is any concern for the patient’s cardiac integrity (very elevated potassium) or if there is uncertainty regarding how quickly the EKG can be acquired or accurately interpreted then there is no reason to delay in giving the calcium gluconate. Keep in mind while this will not lower the patient’s potassium, it is the fastest way to protect the patient (from the lethal consequences of elevated potassium) by stabilizing the cardiac membrane.
Video Tutorial:
To view a video that goes over these orders in the EMR click here.
STEP 3: ACUTE MANAGMENT OF REAL HYPERKALEMIA
The orders that are listed in this section may often times be used however will require a bit more deliberation compared to the orders above (as some of them are not appropriate for all patients and their may be contraindications). Similarly they have been separated by section.
Initiate Appropriate Monitoring For the Patinet:
- Routine BMP draws (Q4H, Q6H, Q12H etc): in certain cases the potassium level will have to be monitored closely. This may change depending on the circumstance but make sure to order some type of interval BMP labs to keep an eye on the potassium levels.
- Glucose monitoring: in cases with concomitant hyperglycemia.
- Telemetry: for patients who are at risk of cardiac issues or have EKG changes the threshold is very low to initiate continues cardiac monitoring.
Improve Renal Excretion Of Potasium:
- Start IV fluids (typically normal saline but exceptions may exist): for patients who may be under resuscitated/pre renal (and do not have contraindications such as being on dialysis or having CHF) starting some IV fluids such as normal saline can help assist in renal excreting potassium.
- Utilize loop diuretics (such as furosemide 20-160 mg): this is often contraindicated in patients with underlying kidney injury as their etiology of hyperkalemia. It may also worsen situations where patients are pre-renal by lowering intravascular volume, HOWEVER it can be effective for quickly eliminating potassium from the body. In patients that are being hydrated well it can be utilized in the right context. It will not be too effective in ESRD patients.
Shift Potassium Intracellularly:
- Dextrose and Insulin: ordering insulin in patients should be performed with caution. Make sure to evaluate the glucose level before ordering insulin however in many cases this is the quickest way to shift potassium intracellularly and acutely lower the potassium level. However this is only a temporizing measure. Typically it is safest to order 50 g of glucose to be given first and then give 10 units of regular insulin after 30 minutes. In other cases (such as those with insulin needs that are not being met, other adjustments can be made to insulin dosing/the patients sliding scale).
Video Tutorial:
To view a video that goes over these orders in the EMR click here.
STEP 4: MORE NUANCED HYPERKALEMIA MANAGEMENT OPTIONS
This section will go over orders that likely will not be required in most patients with hyperkalemia, but should be considered in some of them (and can be useful in some as well).
Close Glucose Control:
- Insulin drip initiation with Q1H glucose checks: in certain patients, a insulin drip will be required to manage their blood sugars and is the safest way to assist in controlling hyperglycemia. Routine (generally Q1H glucose checks will be required). Typically this will mean the patient will need to go to the ICU.
Improve GI Excretion Of Potassium:
- Kayexalate/Sodium Polystyrene (15-30 grams Q4H): this medication is a ion exchange resin that works in the gut to inhibit GI absorption of potassium and causes excretion of potassium out of the IG tract. It will have a slower onset and won’t be ordered immediately for many patients because other more fast acting measures may be sufficient. It is typically used until the patient has enough bowel movements in the context of a normalizing potassium. It is contraindicated in patients who are at high risk for bowel necrosis and perforation (such as those that have had colorectal surgery recently, those with an ileum, those with underlying bowel disease, those with bowel obstructions, etc).
Less Effective Measures Of Shifting Potassium Intracellularly:
- Beta 2 Agonists (10 to 20 mg in 4 mL saline nebulizer over 10 minutes): not the most effective measure of shifting potassium intracellularly, however some data exists to suggests its utility. Seems to have an addictive effect when used with insulin.
- Sodium Bicarbonate (1-2 ampules/ 50-100 meq IV): Typically reserved for patients with CKD and concomitant acidosis. It has the least data to suggest its efficiency.
Hemodyalisys:
- HD: when all else fails, do not forget that the patient can be dialyzed to immediately remove potassium from the serum directly. This also may be one of the initial steps in patient with ESRD who is already dialysis dependent. Make sure to remember that the patient will require some type of dialysis line, such as a temporary dialysis line that can be placed on the floor/the unit.
Video Tutorial:
To view a video that goes over these orders in the EMR click here.
SUMMARY
Page Updated: 06.27.2019