Page Contents
OVERVIEW
Fetal heart rate monitoring is an important tool that can evaluate the heart of the fetus. The ultimate goal of fetal monitoring is to prevent death/morbidity of the fetus due to hypoxia. Hypoxic changes in the fetus will change the fetal heart rate pattern. This justifies the value of the cardiotocogram (CTG)/electronic fetal monitoring (EFM).
It is important to keeping mind that EFM can lead to over diagnosis of fetal distress (and increased rates of Cesarean sections/intervention). This is becasue changes in fetal heart rate patterns during labor are common but significant fetal hypoxia is relatively rare.
BACKGROUND PHYSIOLOGY
The fetal heart has an intrinsic rate that is affected by various factors. The rate of the hear tis reduced by the vagus nerve (parasympathetic) and increased by ether sympathetic response (which can be cause by circulating catecholamines).
COMPONENTS OF CTG/EFM
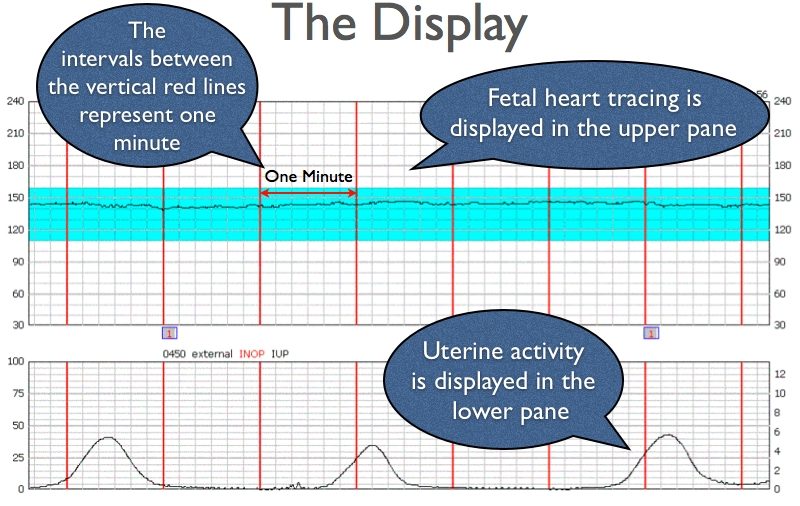
There are two major tracings that are seen on a CTG. The top tracing is the fetal heart rate, while the bottom tracing follows uterine contractions.
SYSTEMATIC INTERPRETATION
As is the case with most things, it is important to have a systematic approach to interpreting results from the CTG. Here is a suggested order of things to evaluate:
Fetal heart rate baseline: one of the first things to appreciate is how fast the fetal heart rate is at baseline. This helps establish context.
Accelerations: these are periods on the tracing where the fetal heart rate increases.
Variability: how variable is the baseline fetal hear rate? Is it fairly constant? Or are there significant alterations?
Decelerations: periods on the tracing were the fetal heart rate decreases.
Contractions: areas on the bottom tracing (for uterine activity) where the uterus is contracting (increased activity).
*Make sure to measure the maternal pulse in because the equipment for CTG can sometimes accidentally measure the maternal rate.
BASELINE FETAL HEART RATE
A baseline fetal heart rate is defined as the average rate over a 10 minute period. It excludes accelerations, decelerations, marked variability, or differences of more than 25 beats per minute (bmp). The rate is rounded to 5 bmp increments, and at least 2 minutes of baseline duration is needed. Normal baselines are between 110 and 160 ppm.
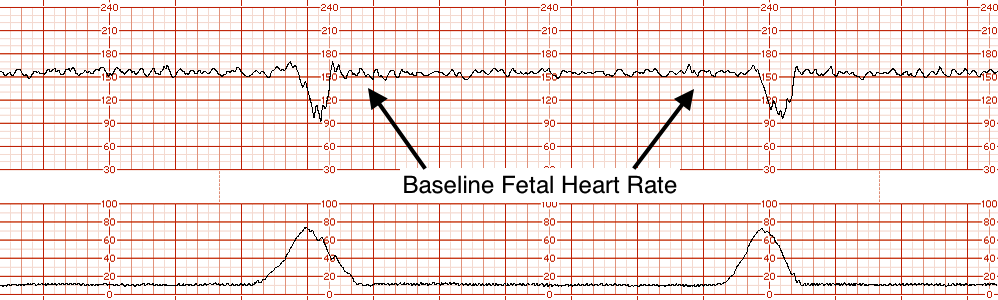
At any point in gestation a rate about 160 bpm should be regarded with suspicion. Make sure to look at long periods of the tracing to make sure you have an accurate impression of the baseline.
The baseline will start to fall a bit as pregnancy advances. It is possible for health term fetuses to have a fetal baseline below 110 due to increased vagal tone.
ACCELERATIONS
Accelerations are increases in the fetal heart rate that are above the baseline by at least 15 bpm. The period of onset to peak is reached within 30 sec in accelerations, and the duration is at least 15 seconds. A acceleration that lasts longer then 2 minute but less then 10 minutes is termed a prolonged acceleration.
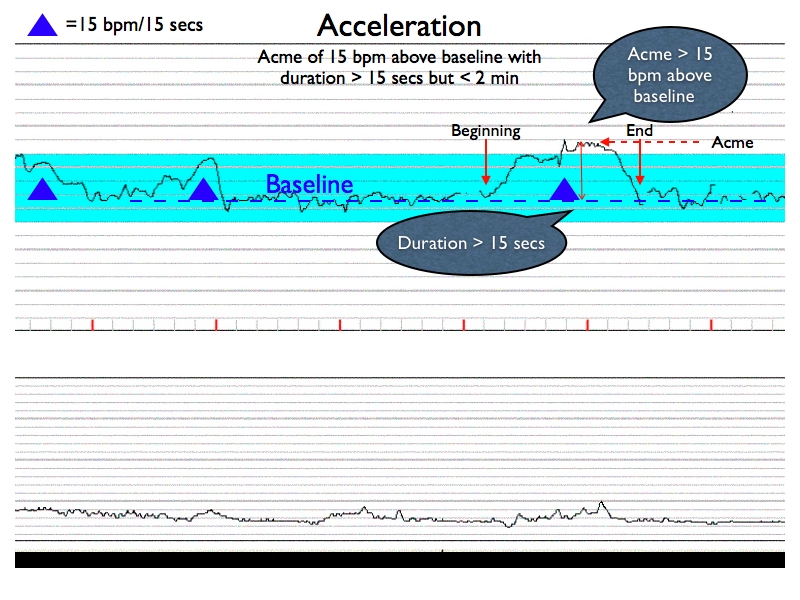
The presence of accelerations on a tracing is good evidence that the fetus is gaining adequate oxygenation. Accelerations occur in relation to the level of central nervous system activity and they tend to accompany fetal movements. As a result, the presence of accelerations is suggestion of a healthy active fetus. With this in mind, there can be benign reasons for the absence of accelerations (such as period of quite sleep for the fetus).
*Ultimately an antenatal tracing should always contain accelerations to be considered normal. Make sure to look at a long enough time period before making this call. A healthy fetus can be in a state of quiet sleep for 40 min (or longer).
*Absence of accelerations over a 60 minute period of time is NOT normal!
VARIABILITY
Variability is defined as the fluctuation of the fetal heart rate above the baseline. Moderate variability is ~ 6-25 bpm. The fetal behavioral state will influence variability.
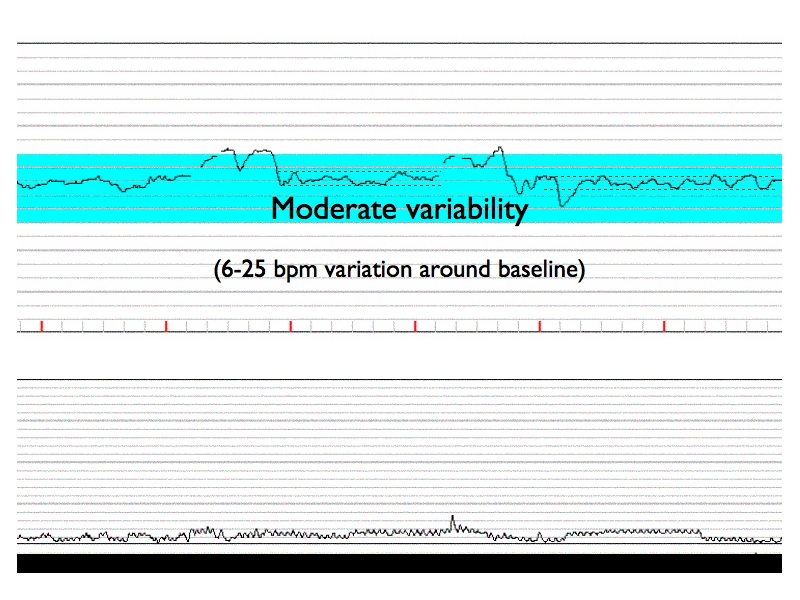
Variability is more accurately displayed using the fetal ECG very. the Doppler ultrasound (which often overestimates variability).
Variability is important to evaluate because it can help evaluate difficult tracings and contextualize decelerations. Moderate variability (even in the setting of deep decelerations) does not suggest significant fetal compromise.
DECELERATIONS:
A deceleration is temporary decrease in the fetal heart rate below the baseline. The can be deep and broad, or sometimes even shallow and subtle. With this in mind, abrupt falls in the fetal heart rate do not count as decelerations.
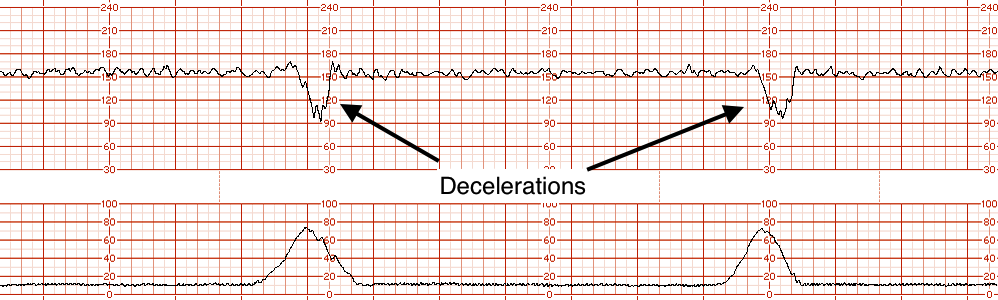
Decelerations are usually a fetal response to stress, and do not necessarily imply hypoxia. The 2 major types of decelerations are:
- Reflex which refers to the activity of the vagus nerve. Hypoxemia can stimulate the vagus nerve and lead to slowing of the fetal heart rate. Transient hypoxemia often occurs during contractions (which can explain why decelerations line up with contractions on the tracings).
- Hypoxia which has a direct effect upon the myocardium. The heart is no longer able to contract effectively because the myocardium is damaged.
*Slow to recover decelerations combined with minimal variability is an ominous sign.
TOCOGRAM
The tomogram measures only the frequency of contractions (not their strength or duration). One can detect tachysystole with a tocogram, which is associated with poor progress in labor. This is because a uterus that contracts too often does not contract appropriately. Furthermore, fetal hypoxia is more likely to occur under such conditions (simply because the fetus has less time in between contractions to recover).
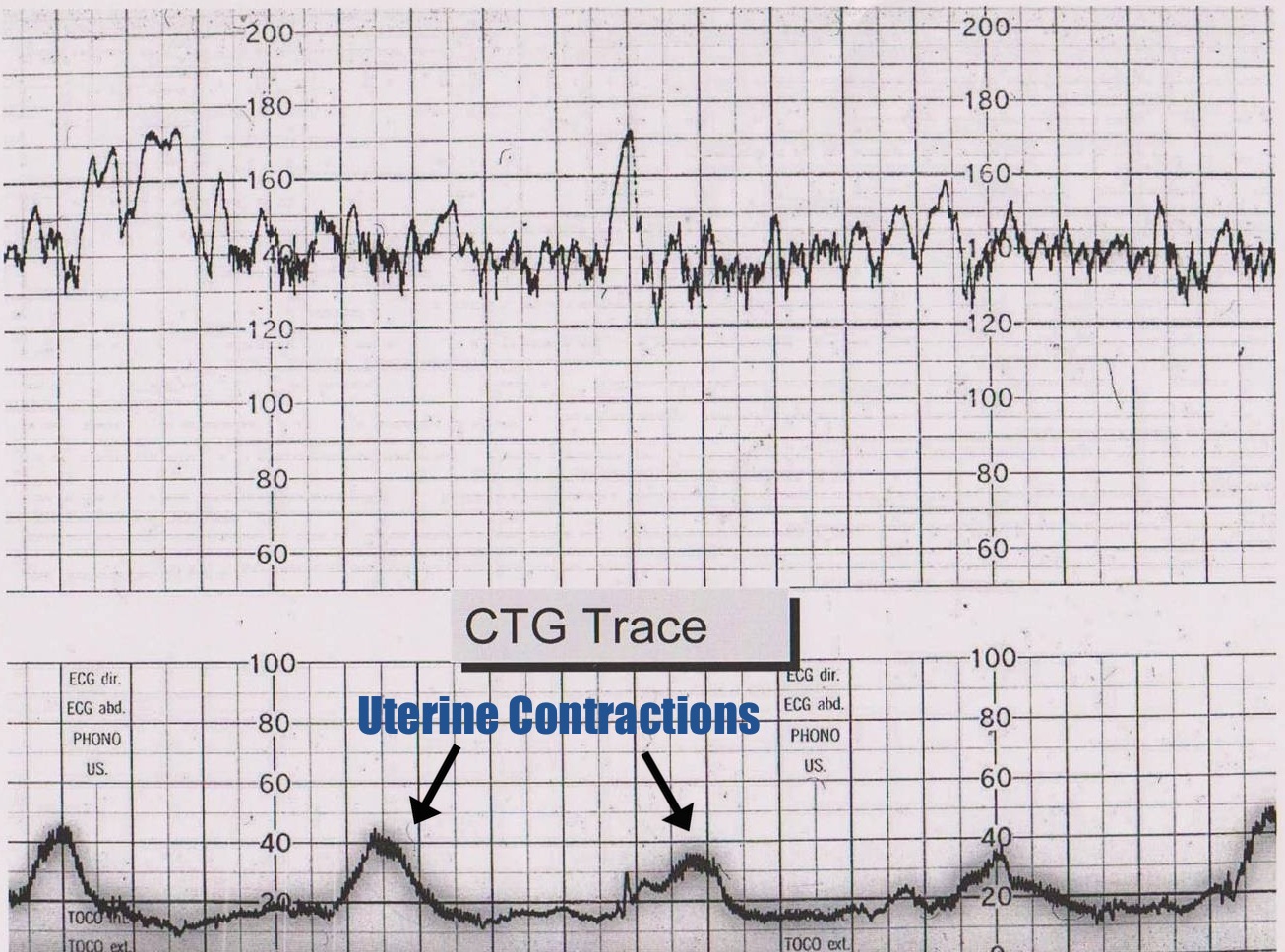
NORMAL TRACING
A normal tracing will be one that has expected accelerative patterns with normal baseline and variability. Such a tracing will give good evidence that he fetus is adequately oxygenated. Typically variability is greater during an active state, and diminished when the fetus is resting.
ABNORMAL TRACING (POSSIBLE HYPOXIA)
Page Updated: 05.01.2016