Page Contents
WHAT IS IT?
Methanol intoxication refers to the unsafe ingestion of the toxic substance methanol.
WHAT CAUSES IT?
Typically it is the accidental ingestion of methanol that causes this to occur. Sources of methanol can be:
- Windshield washer fluid
- Photocopying fluid
- Homemade spirits (such as moonshine)
- Laboratory grade ethanol (to discourage drinking of the ethanol)

WHY IS IT A PROBLEM?
It is the byproducts of methanol metabolism that are the real problem.When methanol is ingested, the enzyme alcohol dehydrogenase (ADH) will metabolize it into formic acid and formaldehyde (i.e. tissue preservative). Formic acid is a dangerous compound in the body because ti binds to cytochrome oxidase and blocks the electron transport chain from functioning. This will cause the body to rely on lactic acid fermentation (leading to lactic acidosis).
Whats more, formic acid also can cause topic nerve damage/retinal damage that can lead to permanent blindness.
WHAT MAKES US SUSPECT IT?
Risk factors
Alcoholism, ingestion of homemade spirits.
Initial Presentation
Presentation will vary deepening on the severity of the ingestion: it can be ether acute or chronic.
Acute poisoning presenting sings/symptoms:
- Mental status changes which can be similar to that of alcohol intoxicaiotn.
- Seizures
- Kussmaul-Klein respirations
- Hypotension
Chronic poisoning patient chief complaints:
- Headache
- Dizziness
- Vision changes/blindness
History Of Present Illness
Often an alcoholic patient will ingest sources of alcohol that are contaminated with methanol.
Physical Exam Findings
HEENT exam:
- Relative afferent pupillary defect may be present and is a bad sign
Fundoscopic exam may reveal:
- Optic disk pallor
- Cherry-red spot in the macula
CLINICAL WORKUP
Basic metabolic panel can show an increased anion gap (metabolic acidosis).
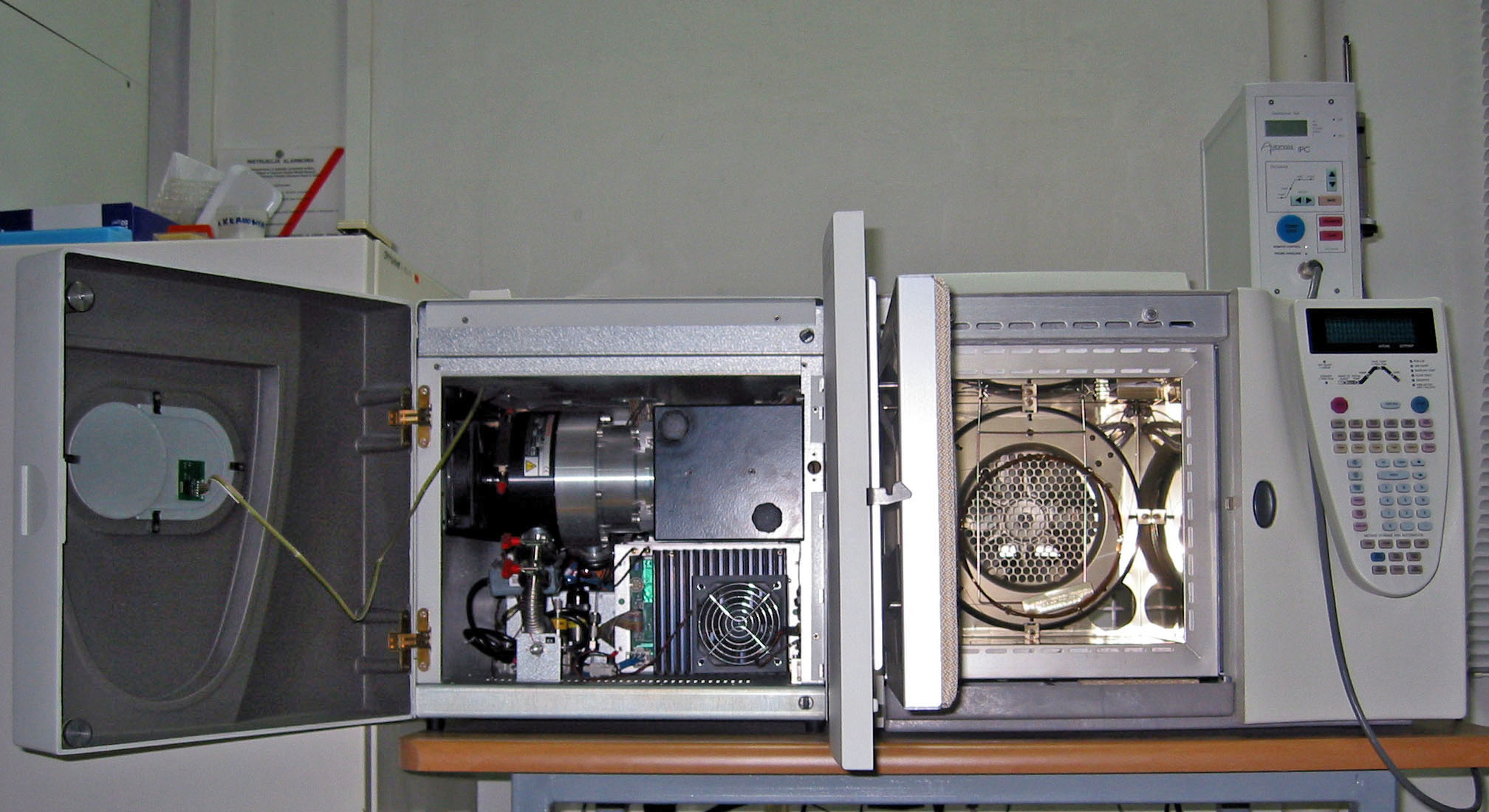
Serum testing for ethylene glycol/methanol levels is often performed by gas chromatography, however such tests are not readily available (and need to be sent out). In many cases patients will be treated for intoxication even without serum confirmation. If the clinical suspicion is high enough, it is not practical to wait to treat the poisoned patient in question.
HOW DO WE RULE OTHER DIAGNOSES OUT?
Fingerstick glucose can be used to rule out hypoglycemia or hyperglycemia
Acetaminophen and salicylate levels (either serum or urine) can be collected to rule out these common coingestions
HOW DO WE TREAT IT?
Goal of treatment is to prevent the metabolism of methanol to avoid toxicity
Fomepizole is an inhibitor of alcohol dehydrogenase and is an antidote for methanol or ethylene glycol poisoning.
Ethanol administration was used before fomepizole became available. This is because ethanol will compete with methanol to bind ADH
Hemodialysis may be needed in more severe cases to rapidly remove the toxin from the blood.
HOW WELL DO THE PATIENTS DO?
This is a potentially fatal condition and requires proper management to preserve the patient’s life.
WAS THERE A WAY TO PREVENT IT?
Avoiding ingesting substances contaminated with methanol is the key to avoiding methanol intoxication.
WHAT ELSE ARE WE WORRIED ABOUT?
Death can occur from untreated methanol toxicity.
Permanent blindness can be caused by direct damage to the optic nerve/retina.
OTHER HY FACTS?
Disulfiram is a acetaldehyde dehydrogenase inhibitor, and would not be effective in treating methanol toxicity.
Methanol is particularly toxic to the striatum, and often tends to involve the pitman and caudate preferentially.
FURTHER READING
Page Updated: 07.25.2016