Page Contents
WHAT IS IT?
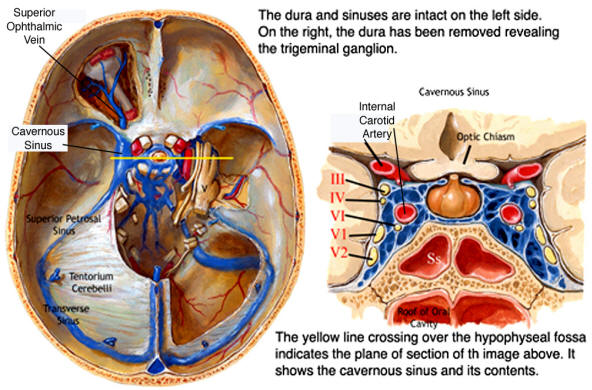
Cavernous sinus thrombosis (CST) refers to the formation or presence of a thrombosis in the cavernous sinus.
WHAT CAUSES IT?
Typically this is caused by an infectious etiology that involves the orbit, nasal sinuses, or central face that then leads to a septic thrombosis of the cavernous sinus. The facial/ophthalmic venous system is valveless, making it much easier for an uncontrolled infection to spread to the cavernous sinus. Staphylococcus aureus is the most common causal pathogen for this condition.
WHY IS IT A PROBLEM?
The spread of an infection to the cavernous sinus can be life threatening and will result in intracranial hypertension due to the impaired venous flow in the orbital veins. This increased intracranial pressure is responsible for the symptoms experienced by patients.
WHAT MAKES US SUSPECT IT?
Risk factors
Orbital, nasal sinus, central face infection.
Initial Presentation
Common Chief Complaints: these are a consequence of intracranial hypertension.
- Headache is the most common presenting symptom
- Seizures
- Nausea/vomiting
- Focal neurological deficits: such as weakness
History Of Present Illness
Headache may be characterized by orbital pain.
Mental status changes such as confusion, drowsiness, and even coma can suggest spread of the infection to the CNS/sepsis
Physical Exam Findings
Vital signs:
- Low grade fever may be present.
Eye exam:
- Decreased visual acuity due to involvement of the optic nerve in this process.
- Diplopia due to cranial nerve dysfunction (can be compressed by cavernous sinus)
- Exophthalmos due to increased intracranial pressure
- Ophthalmoplegia due to cranial nerve dysfunction (can be compressed by cavernous sinus)
- Diminished pupillary responses
Other HEENT exam:
- Periorbital edema can be present due to impaired venous drainage in the cranium.
- Meningismus may be present in later stages of infection.

CLINICAL WORKUP
Complete blood count will demonstrate an elevated WBC count.
Blood cultures for the causal pathogen may identify it in many cases.
Lumbar puncture and CSF studies may show increased pressure.
- Findings may be consistent with either aseptic or frank meningitis.
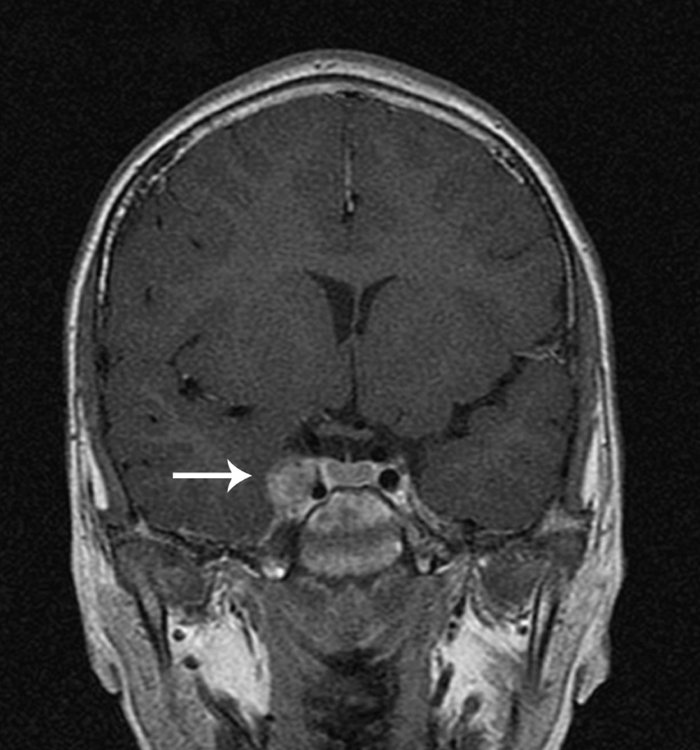
CT scan or MRI might be ordered as part of the initial evaluation: while they can sometimes visualize the thrombosis, if they are normal this does to rule out CST
WHAT ELSE ARE WE WORRIED ABOUT?
Venous hemorrhage: this intracranial hypertension might lead venous bleeding.
HOW DO WE TREAT IT?
Aggressive empiric antibiotic therapy (pending blood culture results) is needed to try and prevent the spread of the infection/death. IV antibiotics are often recommend for 3-4 weeks. The regiment will often include the following (until it can be tailored to the identified organism):
- Penicillinase-resistant penicillin
- Third/fourth generation cephalosporin
HOW WELL DO THE PATIENTS DO?
This is a very serious infection that can be fatal if not treated correctly. Patients who undergo aggressive treatment generally recover without issue.
WAS THERE A WAY TO PREVENT IT?
Avoiding the initial infection in theory could prevent infectious CST form occurring, however this may not always be a practical option.
FURTHER READING
Page Updated: 08.02.2016