Page Contents
- 1 OVERVIEW
- 2 WHAT IS IT?
- 3 WHY IS IT A PROBLEM?
- 4 WHAT MAKES US SUSPECT IT?
- 5 HOW DO WE DIAGNOSE/CHARACTERIZE IT?
- 6 WHAT IS THE FIRST THING TO ASSESS AFTER THE DIAGNOSIS ANEMIA?
- 7 WHAT DO WE ANALYZE IF THE RETICULOCYTE COUNT IS INCREASED?
- 8 WHAT DO WE CONSIDER WHEN AN ANEMIA HAS AN APPROPRIATE BONE MARROW RESPONSE?
- 9 WHAT DO WE CONSIDER WHEN AN ANEMIA HAS AN INAPPROPRIATE/LOW BONE MARROW RESPONSE?
- 10 HOW DO WE FURTHER CHARACTERIZE MACROCYTIC ANEMIAS?
- 11 OTHER TESTS FOR CHARACTERIZATION
OVERVIEW
Some might ask why this topic of Anemia is being covered here separately, and quite frankly anemia is a topic that is often times glossed over in medical school curriculums and not fully explained clearly. There is a logical and practical approach to assessing anemic patients (that has much diagnostic value) that all medical students should be familiar with. Furthermore, anemia can seem complicated if taught poorly (which is not the case!). Use the following guide as a means to teach you how to think critically about analyzing a patient who is anemic.
WHAT IS IT?
Anemia is a very general term that refers to either a deficiency in the number of red blood cells (RBCs) OR the amount of hemoglobin (Hb).
WHY IS IT A PROBLEM?
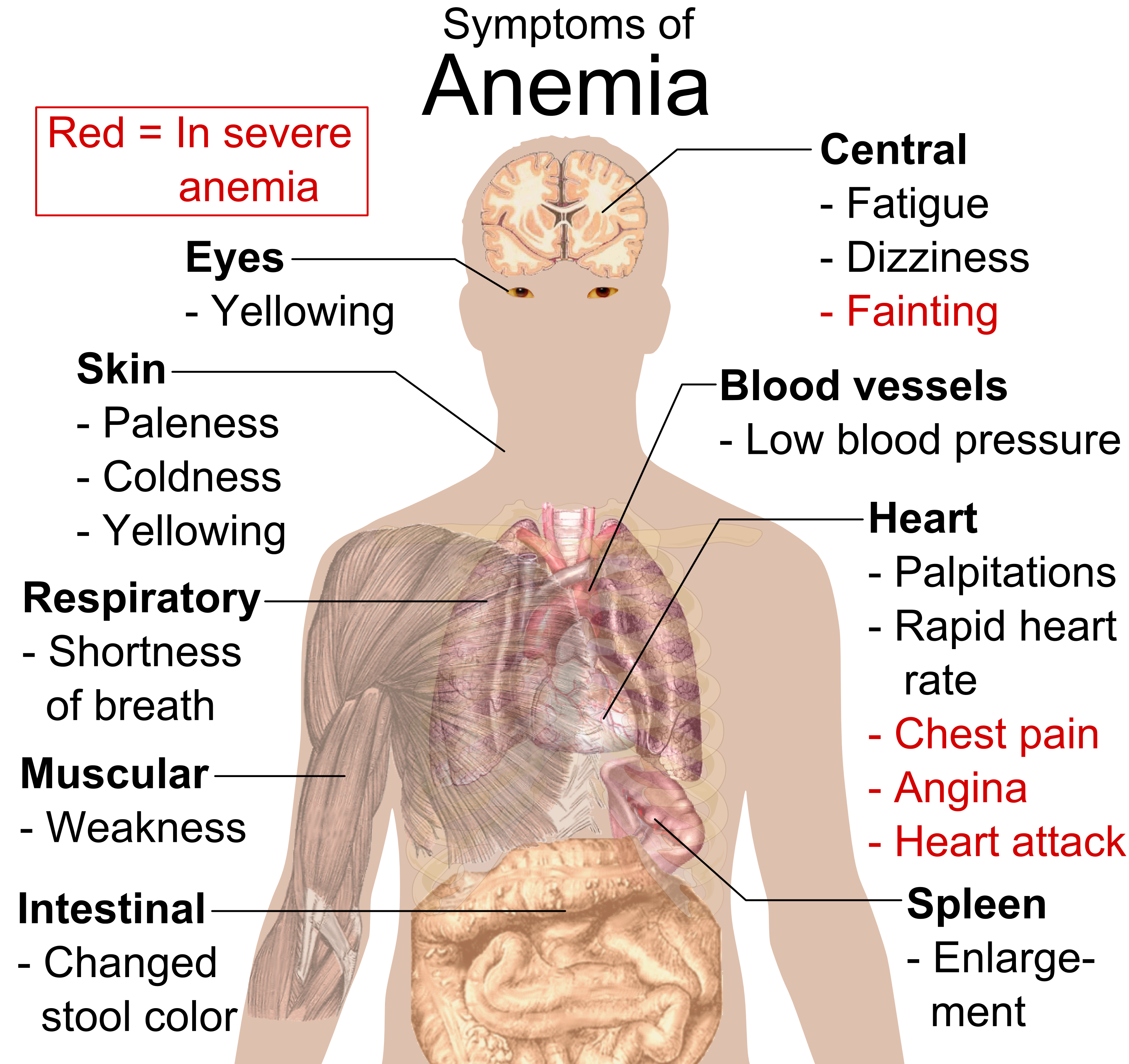
Generally speaking, red blood cells (and the hemoglobin they contain within them) are responsible for transporting oxygen to all of the tissues within the body. As patients become anemic, their ability to deliver oxygen to important tissues (such as the brain, muscles, etc.) becomes compromised.
WHAT MAKES US SUSPECT IT?
Befor delving into the specifics, let us make sure to tie in the above pathophysiology to some of the symptoms of many forms of anemia. In considering issues of oxygen delivery, shortness of breath, fatigue, and dizziness are all classic symptoms of the condition.
HOW DO WE DIAGNOSE/CHARACTERIZE IT?
Given a clinical suspicion of an anemic patient, let us discuss what clinical tools we have at our disposal. Ultimately the Typically one of the initial tests that is ordered clinically (for many different reasons, including suspicion for anemia) is a complete blood count (CBC).
CBC: This test analyzes all of the blood cells, but contains the following information regarding RBCs that is quite relevant for anemia: Hb, hematocrit (Hct), mean corpuscular volume (MCV), RBC count, red blood cell distribution width (RDW), mean corpuscular hemoglobin concentration (MCHC), and mean corpuscular hemoglobin (MCH), and can also include a reticulocyte count.
- Hb: hemoglobin is the most accurate measure of anemia because it assesses the concentration of Hb in the entire blood.
- Hct: this is a calculated percentage that shows what percentage of the blood is made up of RBCs.
- MCV: this measures the average RBC volume (calculated by dividing Hct by the RBC count). Different sizes are used to classify anemias that have small (microcytic), normal (normocytic), or large (macrocytic) sized RBCs.
- RBC count: direct measure of the number of RBCs in the blood (expressed as RBCs per µl of blood).
- RDW: this measures the variation in width of RBCs (and helps contextualize MCV) and can illustrate how uniform RBCs are in their size. An elevated RDW can be caused by certain disorders and is refereed to as anisocytosis.
- MCHC: this is a calculated value that is Hb divided by the Hct. It demonstrates the average concentration of Hb in RBCs. An increase in this value is indicative of certain diseases (such as ones that alter the cell membrane, i.e. hereditary spherocytosis). This value will be decreased in all microcytic anemias (because the RBC volumes are smaller)
- MCH: calculated by dividing Hb by RBC count. This correlates linearly with MCV and has little clinical utility.
- Reticulocyte count: these are immature red blood cells/RBC precursor cells. These will be elevated as the bone marrow produces more RBCs.
WHAT IS THE FIRST THING TO ASSESS AFTER THE DIAGNOSIS ANEMIA?
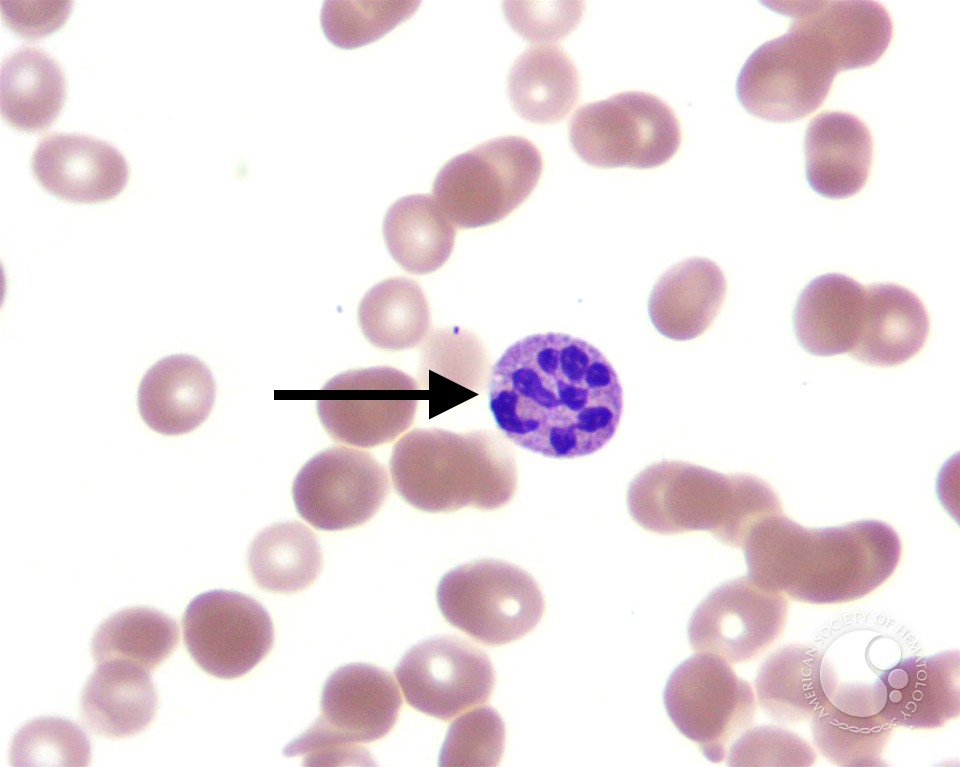
One of the first things to evaluate after noting low Hg/Hct in the a patient is the reticulocyte count (measured as a percentage of total RBC). Reticulocytes are immature/pre-cursor RBCs that normally compose ~1% of the RBC count. These reticulocytes have a reticular (mesh-like) network of RNA that stains with methylene blue on histology.
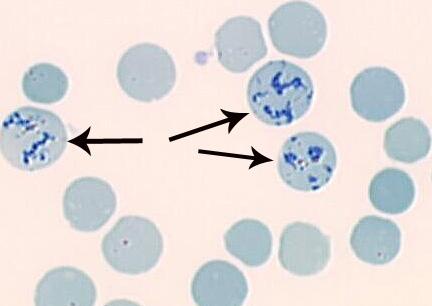
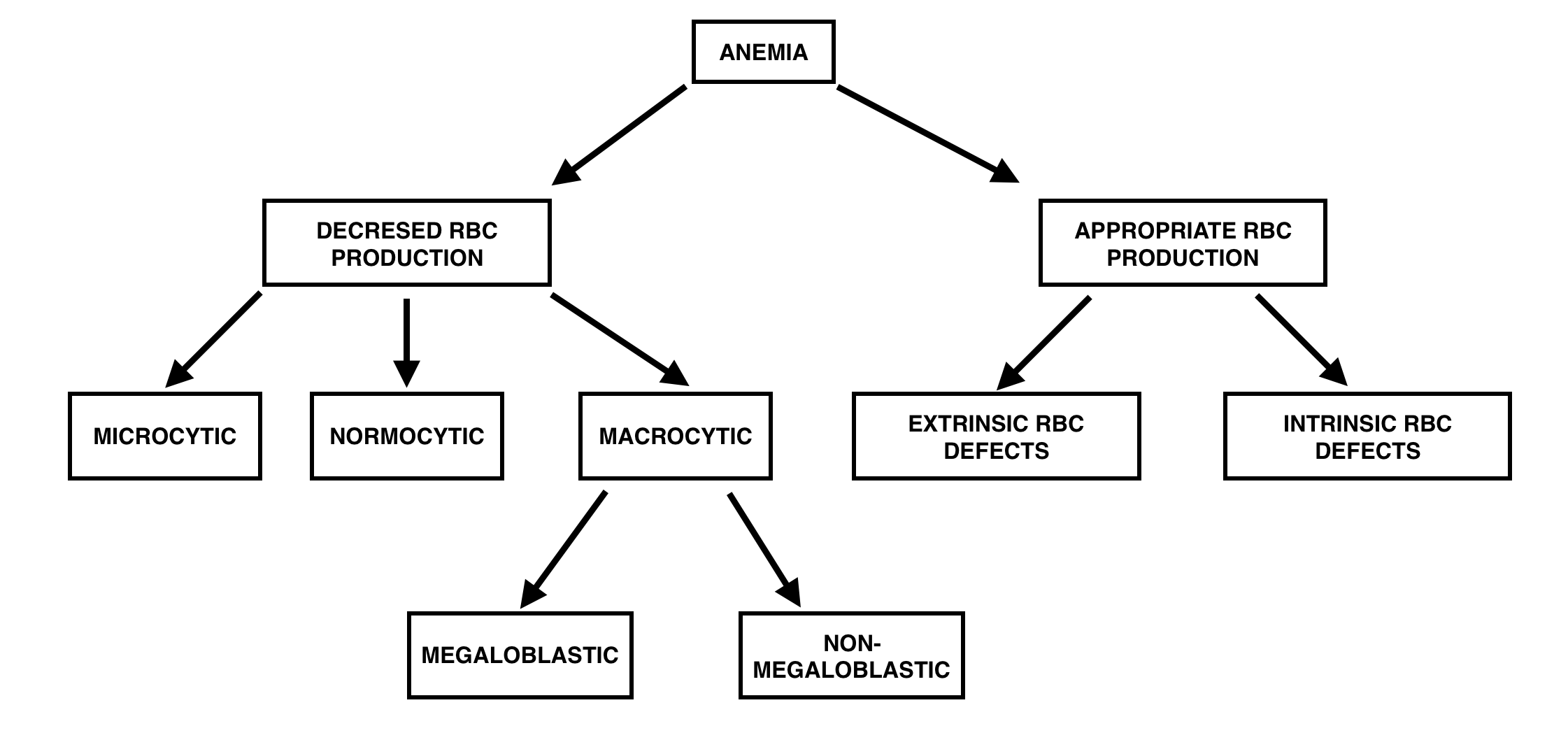
Clinically we refer to this count in order to assess (generally speaking) of the anemia is caused by an issue with the production of RBCs (reticulocytes will be low as a result), or a loss/destruction issue of RBCs (reticulocyte count will be increased as a compensatory mechanism.
WHAT DO WE ANALYZE IF THE RETICULOCYTE COUNT IS INCREASED?
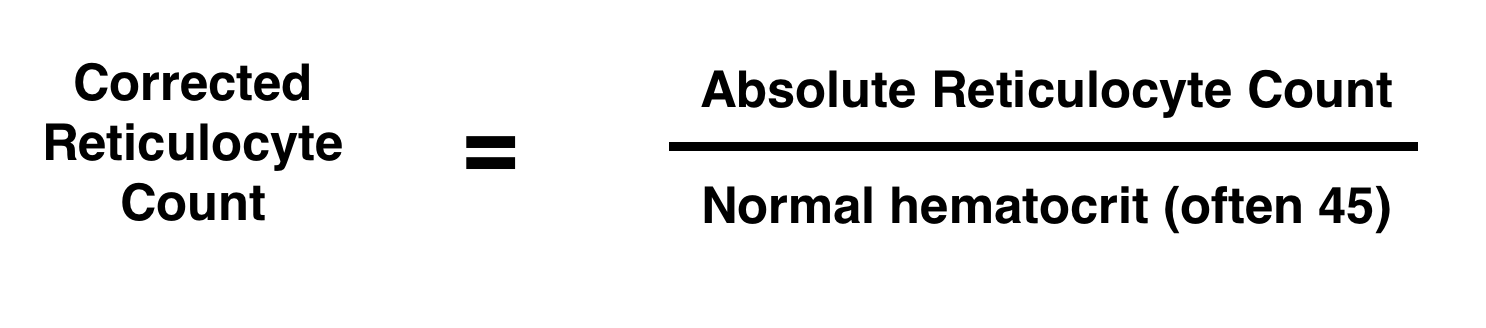
If the reticulocyte count is increased (called anisocytosis in patients the first thing we must do is characterize if this is an appropriate or inappropriate response given the severity of the anemia (essentially this answers the question, is the body doing a good job compensating for the loss/destruction of RBCs?). In order to answer this question we must first normalize the reticulocyte count relative to how sever the anemia is (with a value called the corrected reticulocyte count). The below formula is how this value is calculated.
Generally speaking, an appropriate response to anemia is a corrected reticulocyte count of above 3%.
WHAT DO WE CONSIDER WHEN AN ANEMIA HAS AN APPROPRIATE BONE MARROW RESPONSE?
The two major types of issues that can cause anemia with an appropriate bone marrow response are intrinsic RBC defects (membrane defects, hemoglobin defects, deficient enzymes), or extrinsic RBC defects (hemolytic anemias, blood loss > 1 week, infections). Here are some specific examples of diseases in this category:
Intrinsic RBC defects: hereditary spherocytosis, hereditary elliptocytosis, sickle cell disease, G6PD deficiency
Extrinsic RBC defects: immune hemolytic anemia (warm and cold), microangiopathic hemolytic anemias (HUS, TTP, DIC), malaria
WHAT DO WE CONSIDER WHEN AN ANEMIA HAS AN INAPPROPRIATE/LOW BONE MARROW RESPONSE?
If our reticulocyte count is low (or the absolute value is elevated AND the corrected reticulocyte count is low) then our next step is to assess the size of the RBCs with the patient. This is where the MCV value is very usefully in characterizing anemias as microcytic (< 80 fL ), normocytic (80–100 fL), or macrocytic (> 100 fL ). Macrocytic anemias require further characterization, but let us analyze causes of microcytic/normocytic anemias here:
Microcytic anemias: iron deficiency (later stages) ,thalassemia (alpha and beta), anemia of chronic disease (later stages), sideroblastic anemia, lead poisoning.
Normocytic anemia: anemia of chronic disease (earlier stages), iron deficiency (earlier stages), aplastic anemia (lack of production of RBCs, chronic kidney disease (loss of EPO), invasion of the bone marrow (neoplasms), bone marrow failure
HOW DO WE FURTHER CHARACTERIZE MACROCYTIC ANEMIAS?
If you come across a macrocytic anemia you must then characterize it as either megaloblastic or non-megaloblastic. Megaloblastic refers to specific cellular pathology that can be appreciated histologically, and it is a type of anemia that is caused by inhibiting DNA synthesis during red blood cell production. The pathological state of this anemia is marked by many large, immature, and dysfunctional red blood cells (megaloblasts) in the bone marrow. Also hypersegmented neutrophils will be present (with five or more nuclear lobes).
Megaloblastic anemias: folate deficiency, B12 deficiency (both are required for DNA synthesis)
Non-megaloblastic anemias: liver disease, alcoholism
OTHER TESTS FOR CHARACTERIZATION
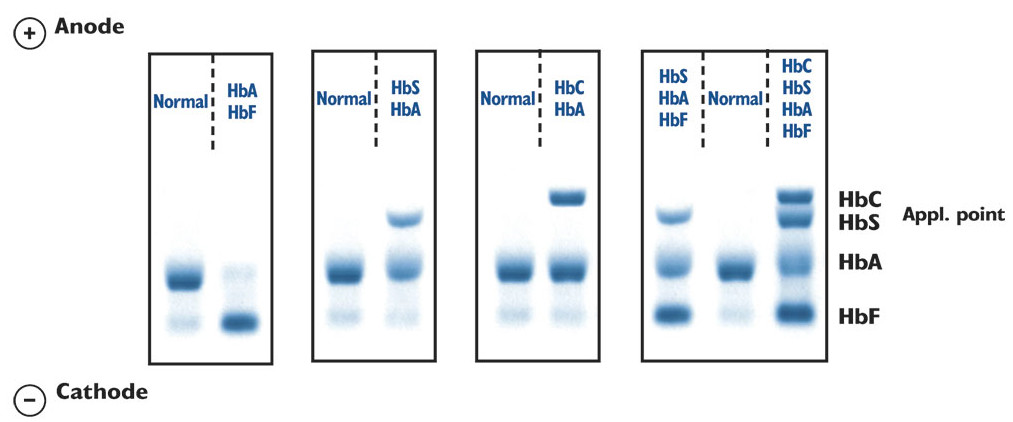
Hb electrophoresis: much like any other type of electrophoresis, this test measures the different types of Hb in the blood and is used in the evaluation of hemoglobinopathies, disorders of Hb structure or synthesis. This is a test that should be ordered only if there is a suspicion of issues directly with hemoglobin.
Haptoglobin: this is a blood plasma protein that binds free Hb released by RBCs during intravascular hemolysis. If you have a clinical suspicion of hemolysis this test can help assess if it is intravascular hemolysis (that occurs within the vessels) or extravascular hemolysis (that occurs by destruction of RBCs in the spleen).
- Intravascular hemolysis: will have increased haptoglobin because Hb will be released directly into the blood.
- Extravascular hemolysis: will have normal haptoglobin values because the RBC’s will be destroyed in the spleen and the released Hb will not be exposed to the circulation (and can not bind haptoglobin).
Page updated: 01.12.2016