Page Contents
OVERVIEW
This guide is dedicated to covering the topic of how to approach treating patients who have hypertension.

WHAT IS HYPERTENSION?
Hypertension at its core is defined as high blood pressure. Specifically, it is most commonly defined as systolic blood pressure (SBP) ≥ 140 mm Hg or diastolic blood pressure (DBP) ≥ 90 mm Hg. With this in mind there are other sub-categorizations of hypertension that are sometimes used.
This elevated blood pressure can serve as a risk factor for many different disease processes, and fundamentally elevated pressure within the vasculature can lead to damage of structures within the body.
WHAT IS THE BASE TREATMENT GOAL?
Given the nature of this condition, its treatment goal is not complicated. Fundamentally the treatment goal involves lowering the blood pressure of the patient to an acceptable level. As is the case with other conditions, there are a finite number of ways that this goal can be achieved.

The role of lifestyle changes: while this element is often glossed over in medicine, it is arguably the most critical.
- Diet: many studies have characterized the impact of salt, alcohol, intake, and other dietary factors as they relate to hypertension.
- Exercise: certain types of exercise have been linked to improvements in blood pressure.
- Other: alcohol, smoking and other lifestyle factors also seem to be associated with the risk of hypertension.
Classes of pharmacological medications:
- Thiazide diuretics
- Calcium channel blockers (CCBs)
- ACE inhibitors (ACEIs)
- ARBs
- Beta-blockers
MAJOR GUIDELINES FOR TREATING HYPERTENSION
Just as is the case with many aspects of medicine, there are many sets of guidelines that have been designed to try guide the clinical management of hypertension. While some are at odds with each other (and many are redundant) we must first become familiar with some of the major guidelines for hypertension before we are able to discuss management.
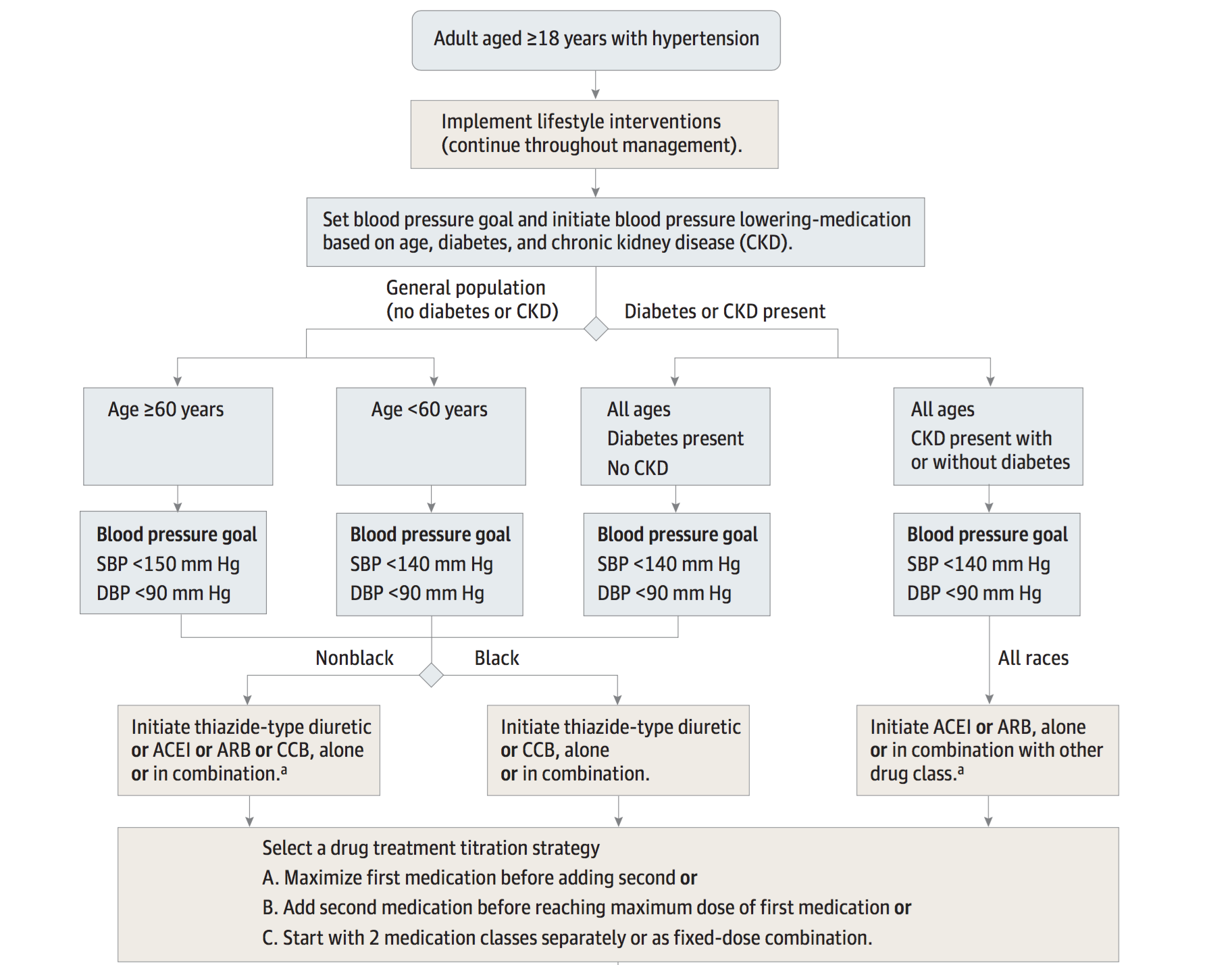
Eighth Joint National Committee (JNC-8): The full report can be found here. However the figure below really helps give some perspective on these guidelines.
INITIAL MANAGEMENT: DECIDING IF LIFESTYLE CHANGES ARE ENOUGH
While it may seem naive to believe that hypertension can be managed with lifestyle change alone, it is important to realize that their ARE instances where medications may be unecassary. This is to say, that not every 18 year old patient who has a blood pressure of 141/90 should begin pharmacological treatment. As a physician, one of the initial decisions that must be made is whether or not lifestyle changes should be tried first with or without supplementary pharmacological management. This decision can be a difficult one to make.
Regardless of what is decided however, it is important to realize that their are lifestyle changes that are strongly associated with lower blood pressure. This topic is summarized very nicely on the American Family Physician website here. With this in mind, there are some important points that are highlighted below.
Dietary Key Points:
- Fruits, vegetables, and whole grains are recommended
- Limiting sodium intake is thought to lower blood pressure
Exercise Key Points:
- Engaging in moderate to vigorous aerobic physical activity multiple times a week is recommended
Other Lifestyle Key Points:
- Limiting/stopping tobacco usage is beneficial
- Limiting alcohol consumption might be of added benefit
INITIATION OF PHARMACOLOGICAL THERAPY: OVERVIEW
While every patient should implement lifestyle changes as a first-line therapeutic measure, it is important to realize that once it is decided a patient needs pharmacological management other factors must be considered to help tailor the treatment to individual patients.

Some other important patient characteristics (that dictate management) include the following:
- Diabetes diagnosis: given the role of diabetes as a risk factor, patients with this diagnosis may have more strict target blood pressures.
- Chronic kidney disease (CKD): some medications will have the added benefit of also managing CKD.
- Age: different age groups sometimes have different target blood pressures (given their risks of different disease processes).
- Race: in the case of hypertension patients are categorized into “black vs. non-black” groups for tailoring treatment.
INITIATION OF PHARMACOLOGICAL THERAPY: PATIENTS WITHOUT DIABETES OR CKD
When starting the path to picking the right medication for patients, it is important to first establish if the patient in question has diabetes or CKD (as this changes a few things). Let us first begin simple and focus on the population of patients who does not have diabetes or CKD.
Medical management: the specific medications that are recommended vary based upon the race of the patient (regardless of their age)
- Non-Black patients: this group of patient can receive a thiazide diuretic, CCB, ACE inhibitor, or ARB.
- Black patients: it is recommended that either a thiazide or CCB medication are used for these patients.
Blood pressure targets: in this population of patients the age of the patient dictates the blood pressure goals.
- Age <60 years: the target is set as an SBP <140 mm Hg and a DBP <90 mm Hg
- Age ≥60 years: the target is set as an SBP <150 mm Hg (a bit more lenient) and a DBP <90 mm Hg
Page Updated: 08.28.2016