Page Contents
- 1 OVERVIEW
- 2 WHAT IS HYPERKALEMIA?
- 3 WHY IS HYPERKALEMIA A PROBLEM?
- 4 WHAT MAKES US SUSPECT HYPONATREMIA?
- 5 HOW IS HYPERKALEMIA DIAGNOSED?
- 6 “PRODUCTION” OF POTASSIUM IN THE SERUM
- 7 CLEARANCE ISSUES OF POTASSIUM: APPRECIATING THE ROLE OF THE KINDEY
- 8 CLEARANCE ISSUES OF POTASSIUM: POOR PERFUSION OF THE KIDNEY
- 9 CLEARANCE ISSUES OF POTASSIUM: COMPROMISED ENaC SYSTEM (POTASSIUM SPARING DIURETICS/IMPAIRED ALDOSTERONE ACTIVITY)
- 10 CLEARANCE ISSUES OF POTASSIUM: DAMAGED RENAL PARENCHYMA
OVERVIEW
This page is dedicated to building a framework for how to approach hyponatremia. This seemingly simple electrolyte disturbance can often become a topic of confusion!
WHAT IS HYPERKALEMIA?
Quite simply, hyponatremia refers to high levels of potassium within the serum. It is defined by potassium levels that are > 5.0 -5.5 mEq/L (although reference ranges may vary depending upon the lab doing the assay).
WHY IS HYPERKALEMIA A PROBLEM?
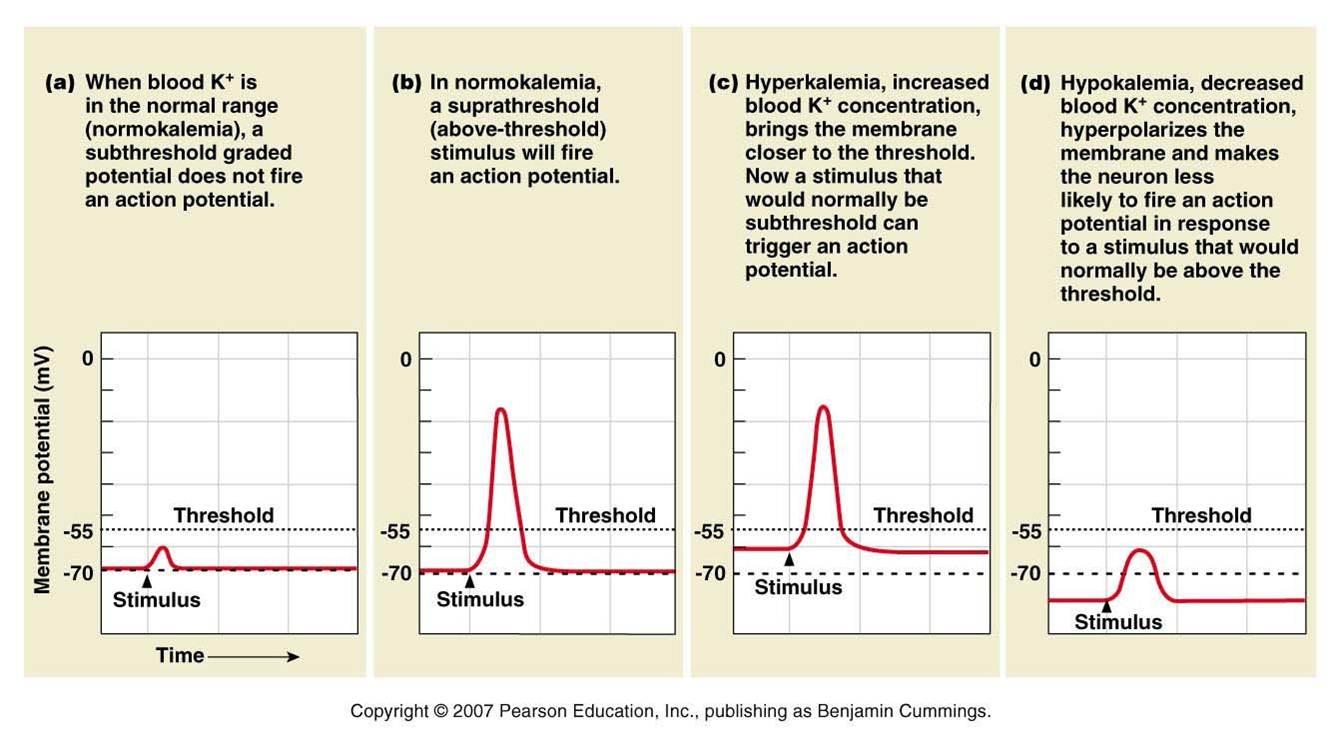
Potassium is an important electrolyte for the function of many different cells and tissues within the body. It is for this reason that a specific concentration of potassium is maintained within the serum. In the setting of hyperkalemia one of the largest clinical concerns is the impact this will have on the heart. Given that cardiac cells rely upon the balance between sodium and potassium to regulate conduction throughout the cardiac system, high levels of potassium will actually impair the ability of the heart to conduct an electrical signal and can lead to arrhythmias. This is because the resting potential of cardiac cells becomes raised in the setting of hyerpkalemia,and cells will depolarize more easily/become inactivated. This becomes a very serious concern as the base function of the heart becomes compromised when it can no longer effectively conduct an electrical impulse throughout its cells/tissues!
WHAT MAKES US SUSPECT HYPONATREMIA?
Risk factors
Acute renal failure, chronic kidney disease, diabetic nephropathy
Presenting symptoms/chief complaints: In reality these are quite nonspecific (however they are worth being familiar with)
- Muscle weakness
- Flaccid paralysis
- Fatigue
Physical exam: generally speaking there are often not clear clinical signs of hypokalemia that will be noticeable on a physical exam.
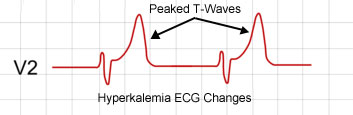
Abnormal EKG findings: this will be discussed more later on, however often times patients are asymptomatic and one of the first signs of an electrolyte disturbance (like hyperkalemia) can be an EKG that shows abnormalities. Look here for more information on this topic.
HOW IS HYPERKALEMIA DIAGNOSED?
The formal diagnosis of hyperkalemia is made from measuring serum potassium (from a test such as a basic metabolic profile). Once this diagnosis is made, we need to have a methodology for discovering what is causing hyperkalemia in our patient.
It is important to realize that while hyperkalemia can be diagnosed from the serum value, its cause can not. Because the differential for hyperkalemia is broad, we must break it down into categories that each have their own clinical workup. A broad overview of this is shown in the figure below that highlights how hyperkalemia truly can be thought about in terms of “production” and “clearance”.
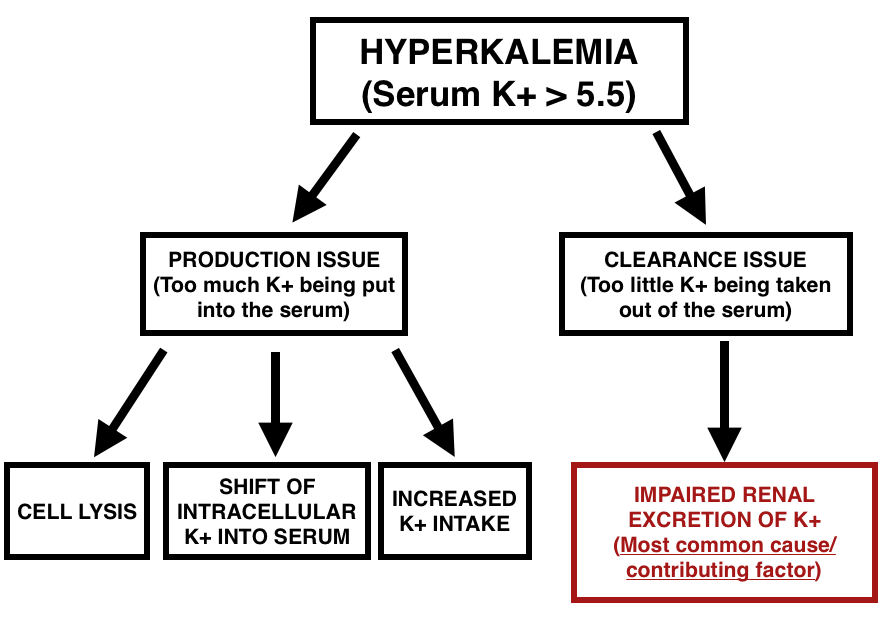
IN REALITY HYPERKALEMIA CAN BE MULTIFACTORIAL AND CAN INOLVE MORE THEN ONE PROCESS
“PRODUCTION” OF POTASSIUM IN THE SERUM
Going in the most intuitive order possible, when thinking about potassium handling in the body (and its implications on hyperkalemia) we must appreciate that there are a finite number of ways in which the potassium levels can be elevated in the serum.
Increased potassium intake: while this is not the major contributing factor for most cases of hyperkalemia, we must appreciate that most all of the potassium in the serum of a patient initially was found in their diet. Fundamentally if too much potassium is being taken in by the body, this can cause elevated levels of serum potassium. While this may be difficult to accomplish by dietary means alone, clinically IV fluids (such as Ringer’s lactate) can be a source of additional potassium.
Cells lysis: given that there is a high concentration of potassium within cells (due to the role of intracellular potassium in maintaining membrane potentials), processes by which cells within the body are lysed will increase serum levels of potassium.
Some examples of disease processes that can cause hyperkalemia by cell lysis include:
- Hemolytic anemias
- Tumor lysis syndrome
Shift of intracellular potassium into the serum (not by cell lysis): it is important to appreciate that short of cell’s lysing (and releasing all of their intracellular potassium into the serum) that there are other physiological mechanisms within the body by which intracellular levels of potassium can be released into the serum (causing hyperkalemia). Some examples of this include:
- Acidemia: high levels of H+ in the serum of patients will encourage cells within the body to exchange a serum hydrogen ion for an intracellular potassium ion. While this mechanism will raise the pH of the serum, it comes at the cost of also raising the serum levels of potassium ions.
- Low insulin activity: insulin increases the cell’s permeability to potassium (by increasing the activity of the sodium-potassium pump). It is for this reason that in situations of low insulin activity patients will have a shift of potassium out of cells and into the serum (the less the sodium-potassium pump works, the more potassium will remain in the serum).
CLEARANCE ISSUES OF POTASSIUM: APPRECIATING THE ROLE OF THE KINDEY
In thinking about how potassium is handled in the body, let us appreciate that potassium can be lost in the sweat, vomit, feces, and urine of the patient. In thinking about which organ is generally charged with regulating potassium levels within the serum, we realize the unparalleled importance of the kidney. Most cases of hyperkalemia involve the kidney in some way simply because the kidney is normally charged with compensating for many of the contributing factors of hyperkalemia listed above (i.e. even if you eat many bananas daily you normally do not become hyiperkalmeic because the kidney will remove excess potassium in your urine). To simplify let us keep in mind that one of the major roles of the kidney is to remove potassium from the serum, and excrete it in the urine. Any process that undermines the kidney’s ability to do this will contribute to increased levels of potassium within the serum.
Taking a look at the figure below helps us develop a framework for how we should approach the broad topic of impaired renal excretion of potassium.
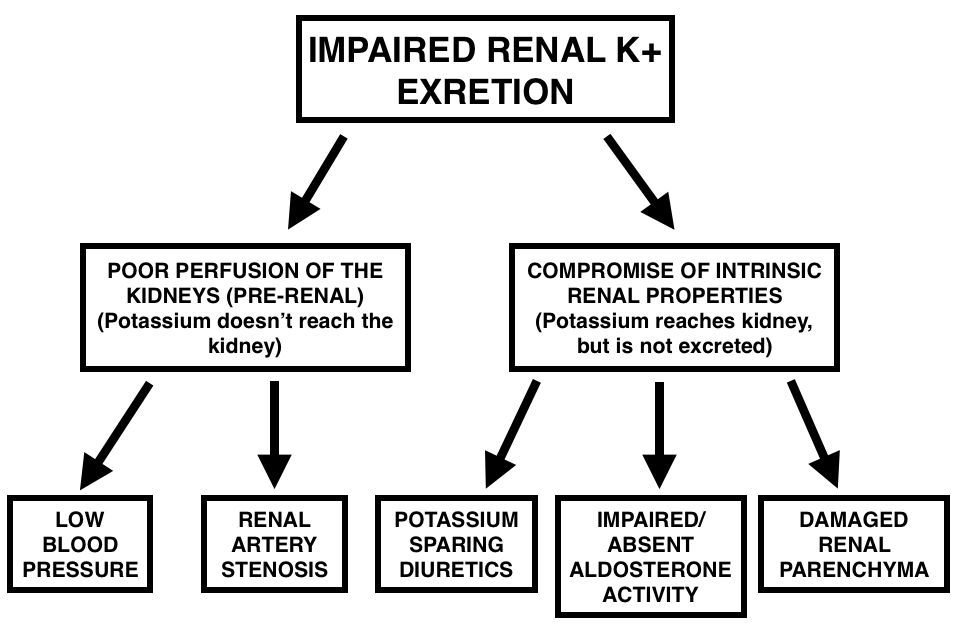
CLEARANCE ISSUES OF POTASSIUM: POOR PERFUSION OF THE KIDNEY
It is important to understand that even if the kidney is completely healthy and functional, it can not excrete serum potassium into the urine if it is not receiving appropriate blood flow. To put it in the form of a fundamental question “How can the kidney excrete potassium if the potassium in the serum never makes it to the kidney?”. The short answer to this question is that the kidney can not excrete potassium under these circumstances! Pre-renal azotemia is used to describe this state of renal hypo-perfusion and can be caused by a variety of processes.
- Hypotension: if the blood pressure of the patient drops too low, they will be unable to delivery enough blood to the kidneys.
- Renal artery stenosis: if mechanical processes obstruct blood flow to the kidneys, this can also contribute to a state of renal hypo-perfusion.
CLEARANCE ISSUES OF POTASSIUM: COMPROMISED ENaC SYSTEM (POTASSIUM SPARING DIURETICS/IMPAIRED ALDOSTERONE ACTIVITY)
To talk specifics, it is the epithelial sodium channel (ENaC) within the kidney that is the “workhorse” when it comes to excreting potassium in the urine. Found primarily in the distal convoluted tubule, the ENaC is responsible for resorbing a sodium ions from the kidney filtrate (which in turn promotes the net efflux of potassium ions into the urinary filtrate). It is important to appreciate that the hormone aldosterone is very critical to the function of the ENaC channel.
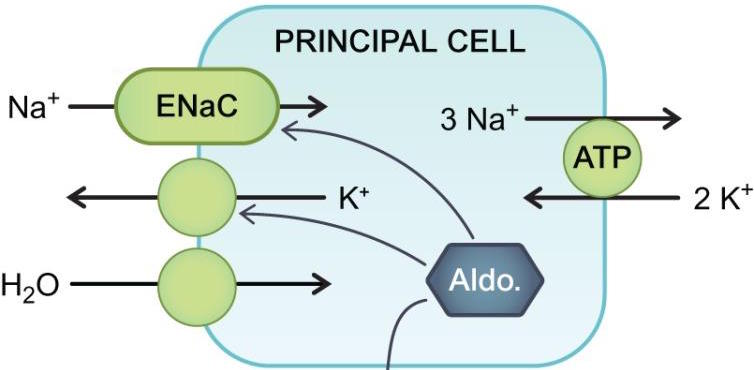
Any process that compromises the function of this channel (either directly, or through aldosterone). will result in decreased urinary loss of potassium (and increased levels of potassium in the serum). Some specific examples of this include:
- Potassium sparing diuretics such as Spironolactone is a competitive aldosterone receptor antagonist that decrease ENaC activity
- Loss of aldosterone through disease processes such as congenital adrenal hyperplasia and Addison disease will contribute to hyperkalemia in a similar manner.
CLEARANCE ISSUES OF POTASSIUM: DAMAGED RENAL PARENCHYMA
While there can be many examples of how the kidney tissues can become damaged, fundamentally the goal of this section is to impress upon everyone that regardless of the CAUSE of kidney damage, if the kidney’s functional ability to perform its normal functions becomes compromised, this very often will result in elevated serum levels of potassium.
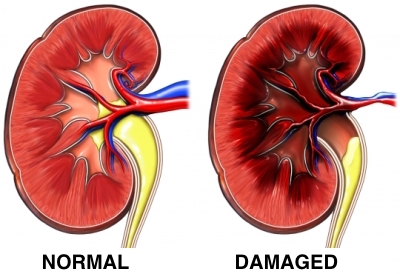
Some specific examples of this can include:
- Acute kidney injury
- Chronic kidney disease
- Diabetic nephropathy
Page Updated: 08.30.2016