Page Contents
WHAT IS IT?
Cold autoimmune hemolytic anemia/warm immune hemolytic anemia (CAHA/CIHA) occurs when autoantibodies within the body target host red blood cells. CAHA is caused by cold reactive IgM auto-antiboides that have optimal activity against red blood cells and at 4°C (cold agglutinin syndrome). This is a type II hypersensitivity reaction that can occur as a response to certain infections (such as Mycoplasma pneumonia and infectious mononucleosis). Many cases are also idiopathic.
WHY IS IT A PROBLEM?
The targeting of these red blood cells (RBCs) by autoantibodies will ultimately cause their destruction leading to hemolytic anemia, and diminished oxygen carrying capacity within the blood. This IgM mediated disease usually causes intravascular hemolysis becasue it fixes complement after binding RBCs causing destruction of the cell within the vessels.
WHAT MAKES US SUSPECT IT?
Risk factors: Lymphoproliferative disorders (i.e. lymphoma/leukemia), immune diseases.
Chief Concern: fatigue, breathlessness, dizziness (symptoms of anemia)
Dark urine: this may occur if hemoglobin is present in the urine (hemoglobinuria)
Skin: may be pale (due to anemia) or jaundiced (due to hemolysis)
HOW DO WE CONFIRM A DIAGNOSIS?
Complete blood count (CBC): demonstrates normocytic or macrocytic anemia, increased red cell distribution width (RDW), increased reticulocyte count, elevated lactate dehydrogenase, and increased indirect bilirubin may all be present (in different combinations). These all suggest a hemolytic anemia and can support the diagnosis of autoimmune hemolytic anemia.
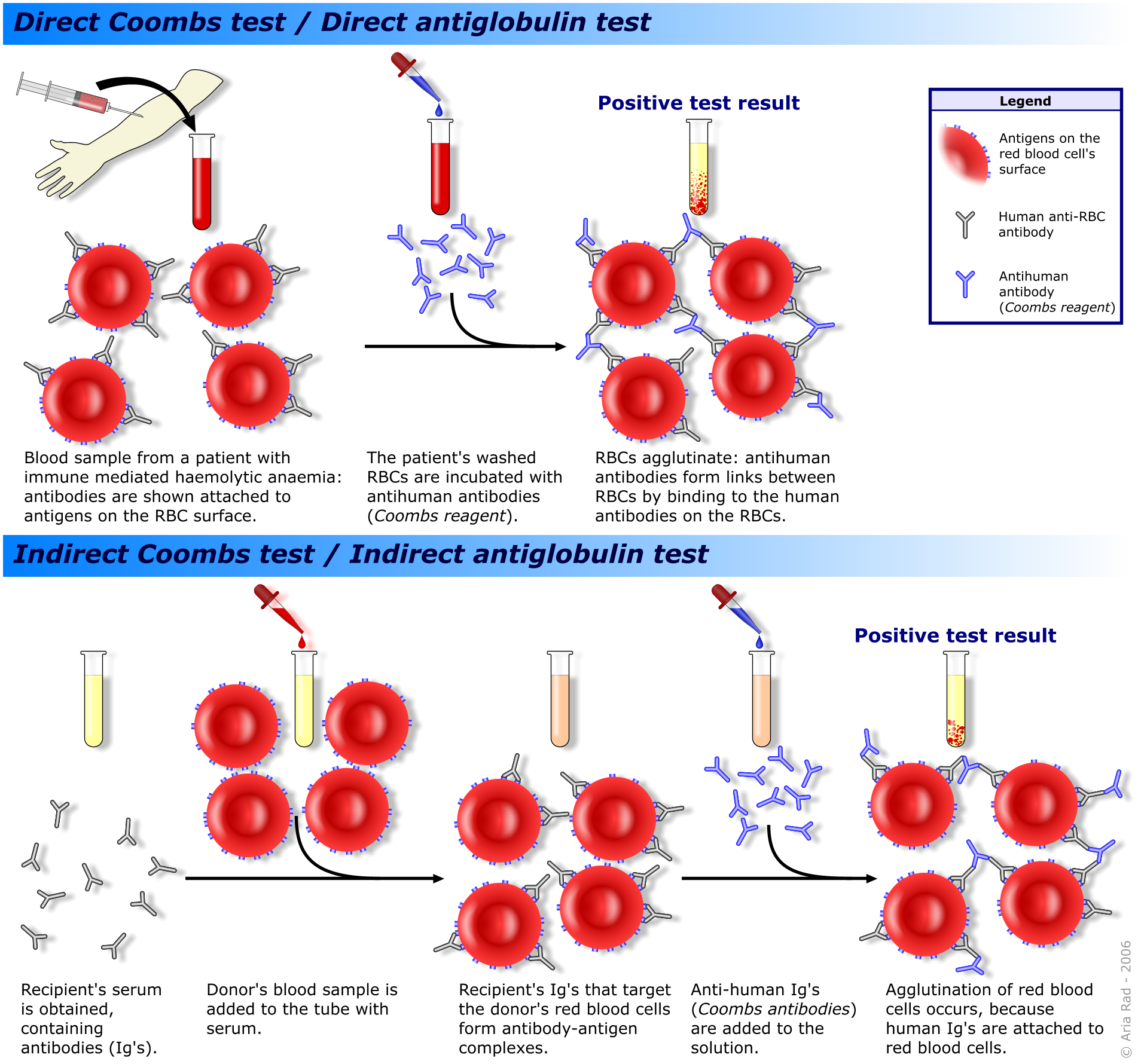
Positive direct Coombs test: in cold AHA patient sample will be positive for direct coombs test (using anti complement antibodies). It should not be positive when using an IgG antibody (the absence of positive IgG coombs test can rule out warm autoimmune hemolytic anemia).
HOW DO WE TREAT IT?
*Blood transfusion may be needed acutely in sever cases until hemolysis can be controlled. WARM THE BLOOD FOR PATIENTS WITH CAHA PRIOR TO ADMINISTRATION
*Avoiding cold temperatures often first treatment strategy!
Rituximab: considered first-line treatment for cold agglutinin disease that requires treatment. Monoclonal antibody that targets CD20 (found on B-cells).
Therapeutic plasma exchange (TPE) may be indicated as second-line therapy for severe cold agglutinin disease. In this procedure patient blood is removed, the disease causing antibody removed (by filtering and discarding the patients initial plasma), then returning the RBCs to the patient with donor plasma or albumin.
*Splenectomy and steroids are not thought to be effective treatments in light of the possible options above
HOW WELL DO THE PATIENTS DO?
Variable prognosis, some idiopathic condense are chronic and stable lifelong, other more acute/paroxysmal attacks of hemolysis rarely recur (source).
WAS THERE A WAY TO PREVENT IT?
Avoiding cold temperatures can sometimes be a treatment strategy for this condition, and will prevent the autoimmune destruction of RBCs.
WHAT ELSE ARE WE WORRIED ABOUT?
This condition can be seen in patients with chronic lymphocytic leukemia (CLL). Addressing a possible clinical suspicion of these conditions might be beneficial.
OTHER HY FACTS?
Cephalosporins can cause immune hemolytic anemia
Page Updated: 01.08.2016