Page Contents
OVERVIEW
This page is dedicated to covering a very important call case: a basilar thrombus. This page will specifically cover this diagnosis in the setting of making the finding on CTA imaging. In many cases a CTA is acquired as part of a “code stroke” CT protocol which also includes non-contrast and perfusion imaging.
This page will focus primarily on CTA findings however this page will also touch on some non-contrast imaging as well.
WHAT IS IT EXACTLY?
A basilar thrombus is exactly as it sounds: it is a thrombus within the basilar artery. This is typically an acute condition and is often an occlusive thrombus. With this in mind it can involve any portion of the basilar artery: sometimes the thrombus is only at the tip of the vessel (basilar tip thrombus), however sometimes it can involve the entire vessel (as seen in the case above).
WHY IS IT AN IMPORTANT CALL CASE?
A basilar thrombus is an INCREDIBLY time sensitive call case (every minute counts) because the basilar artery typically supplies all the posterior blood circulation to the brain, as well as key portions of the brainstem. Once this vessel is occluded patients can have very debilitating neurological deficits which can be lethal if left untreated.
A basilar thrombus is classified as a large vessel occlusion (LVO) and can be treated with embolectomy (more on this below). The success of treatment depends entirely on the time to intervention, which is greatly informed by the time to imaging diagnosis. The sooner this diagnosis is made, the higher likelihood the patient will receive a life changing intervention.
WHAT CLINICAL CONTEXT HELPS RAISE SUSPICION FOR THIS DIAGNOSIS?
A variety of neurological deficits can be seen in the setting of basilar thrombus:
- Posterior circulation related changes: vision changes, dizziness
- Other neurological deficits (some brainstem related): motor deficits, hemiparesis or quadriparesis, facial palsies, headache, and speech abnormalities.
- Severe cases can present as “Locked in Syndrome” from brainstem injury: complete paralysis of all voluntary muscles except for the ones that control the movements of the eyes.
WHAT IS THE KEY TO MAKING THIS DIAGNOSIS ON CALL?
There are two major categories of findings that can be made on CT imaging: non contrast brain findings, and CTA findings. These (and the cases in the archive below) are covered in the following video:
Non-Contrast Brain CT Findings – “Hyperdense” Basilar Artery: this findings is very subtle and its sensitivity/specificity is yet to be established. That being said sometimes this finding is present and is the only clue that the patient has a basilar thrombus. The finding is really just a dense basilar vessel on a non-contrast head CT (as shown below). This is why it is useful to trace vessels on your non-contrast brain CT search pattern.
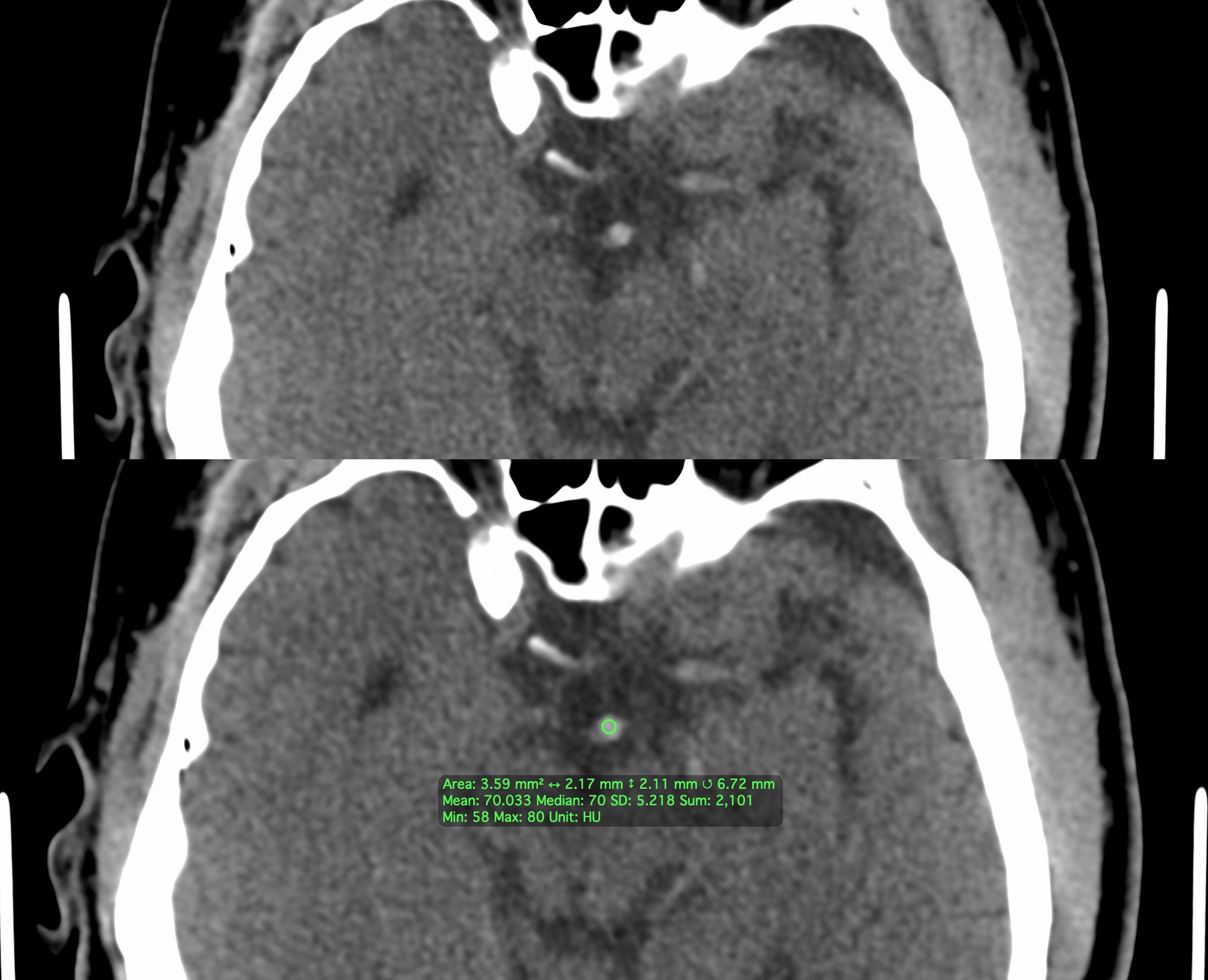
The above image shows an example of a hyper-dense basilar artery which turned out to be an acute thrombus. There is no true density cutoff however if the basilar artery seems brighter than expected its important to consider if the patient may have a basilar thrombus. Measuring the mean and maximum density of the vessel can be useful (in the example a mean of 70 HU and maximum of 80 HU is concerning). At the end of the day if the basilar artery seems dense (and the patient is not already about to get vessel imaging) call the ordering provider to corroborate and discuss if the patient is at risk for a basilar thrombus. In the absence of any true neurological symptoms may truly be nothing, however it is worth confirming this before blowing off the finding given how devastating a delayed/missed diagnosis can be to the patient.
CTA Brain Findings – Filling Defect of the Basilar Artery: this is the actual gold standard for making this diagnosis. If there is a true filling defect seen in the basilar artery this is essentially diagnostic of a basilar thrombus. In some cases it is possible that this could be advanced atherosclerosis, however in most cases (especially in the absence of prior imaging) it is important to treat most all filling defects in the basilar artery as a serious and time sensitive basilar thrombus.
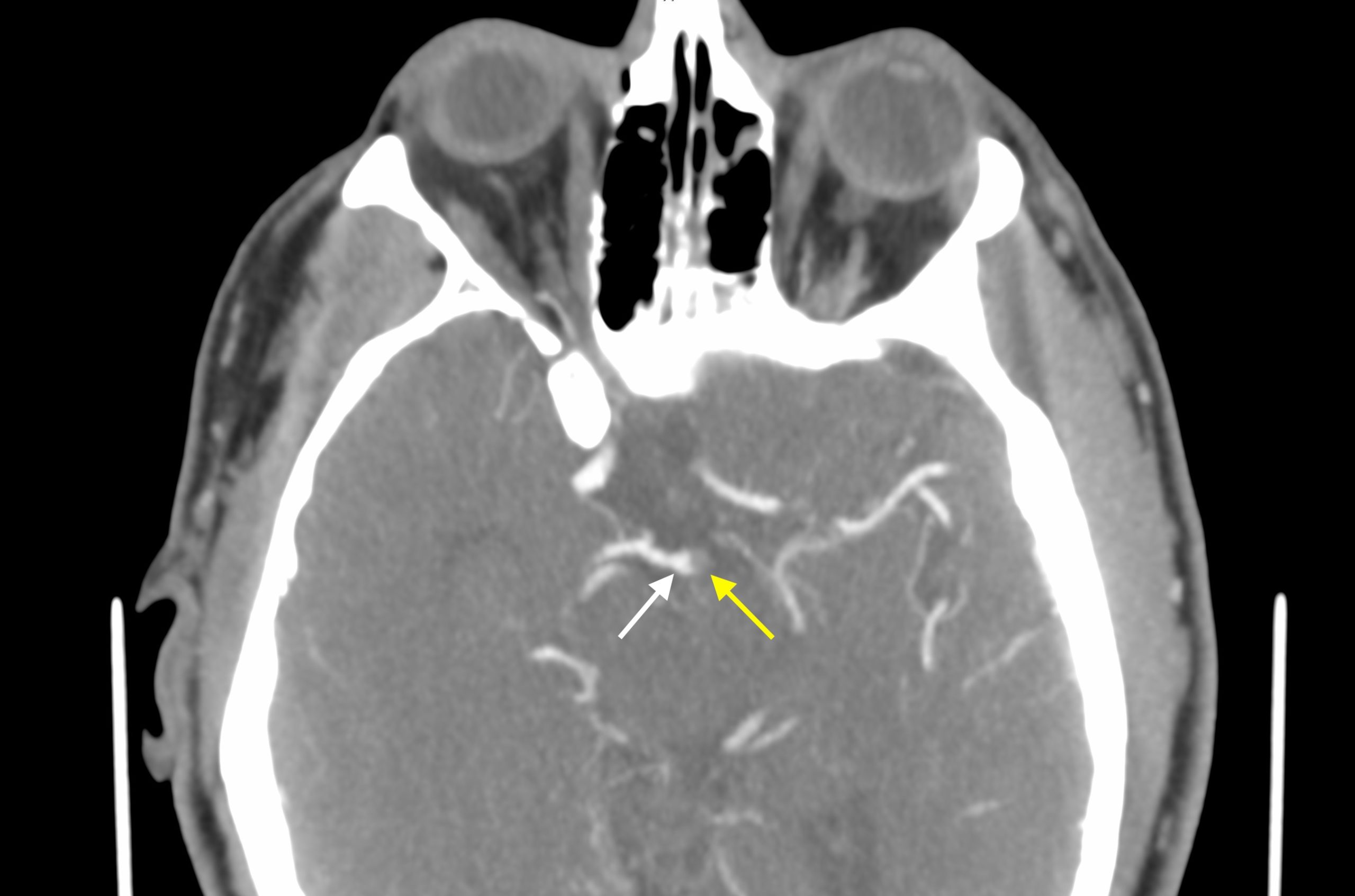
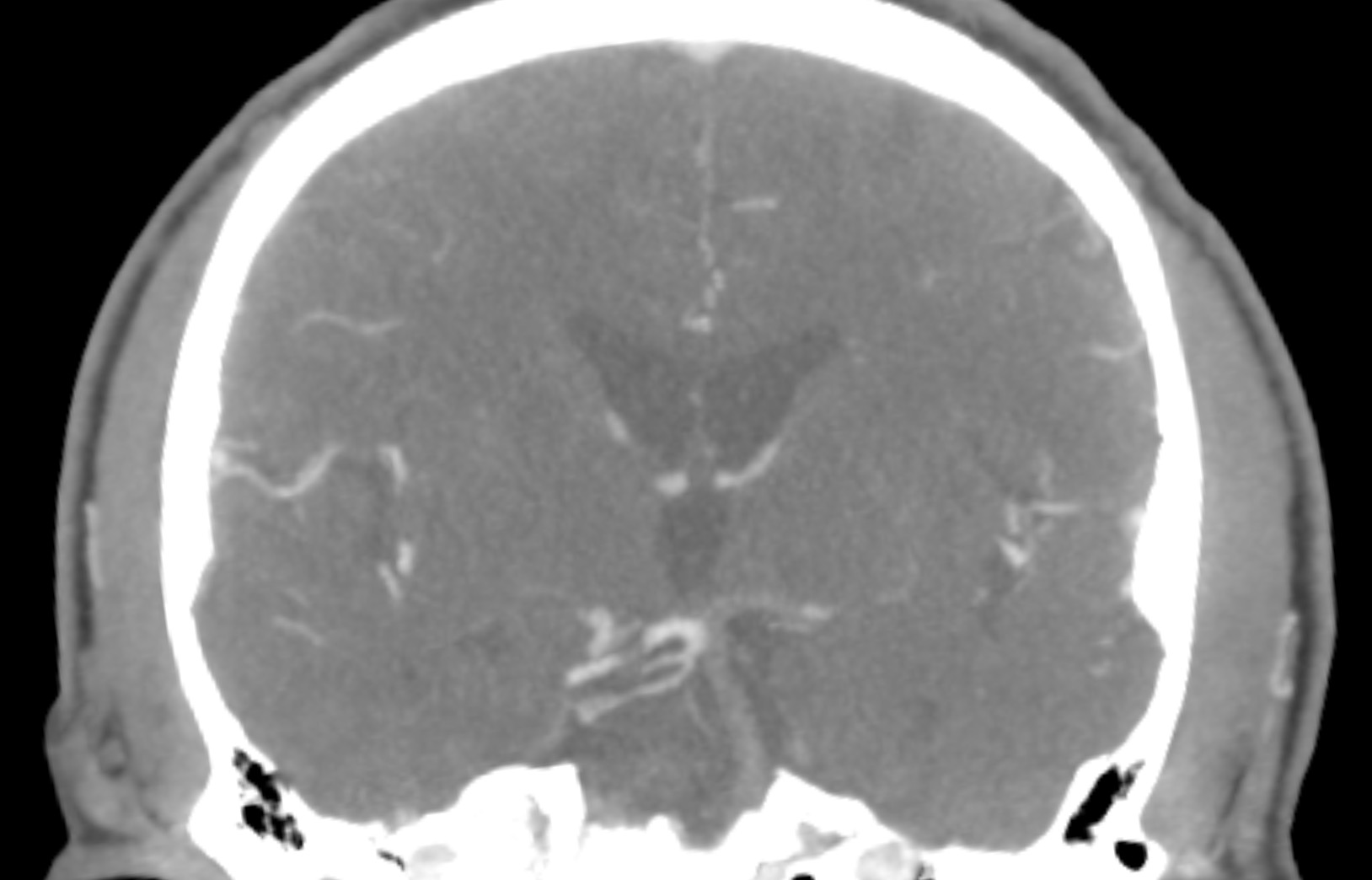
Given that the density of the clot is sometimes increased (hyperdense) it is important to not let delayed post contrast imaging fool you into thinking the vessel is opacified. Sometimes the dense clot is bright enough to mimic the density of a vessel with delayed contrast. Additionally the coronal images are very useful for evaluating the length of the basilar artery as some basilar tip thrombi can be almost hidden on axial images (and are much more apparent on coronal reformats).
WHAT HAPPENS NEXT AFTER THE DIAGNOSIS IS MADE?
If the patient is in the appropriate treatment window, and resources are available, the patient will be rushed to the neuro-interventional radiology suite so an embolectomy can be performed. If successful the occlusion can be resolved and the patient can regain neurological function.

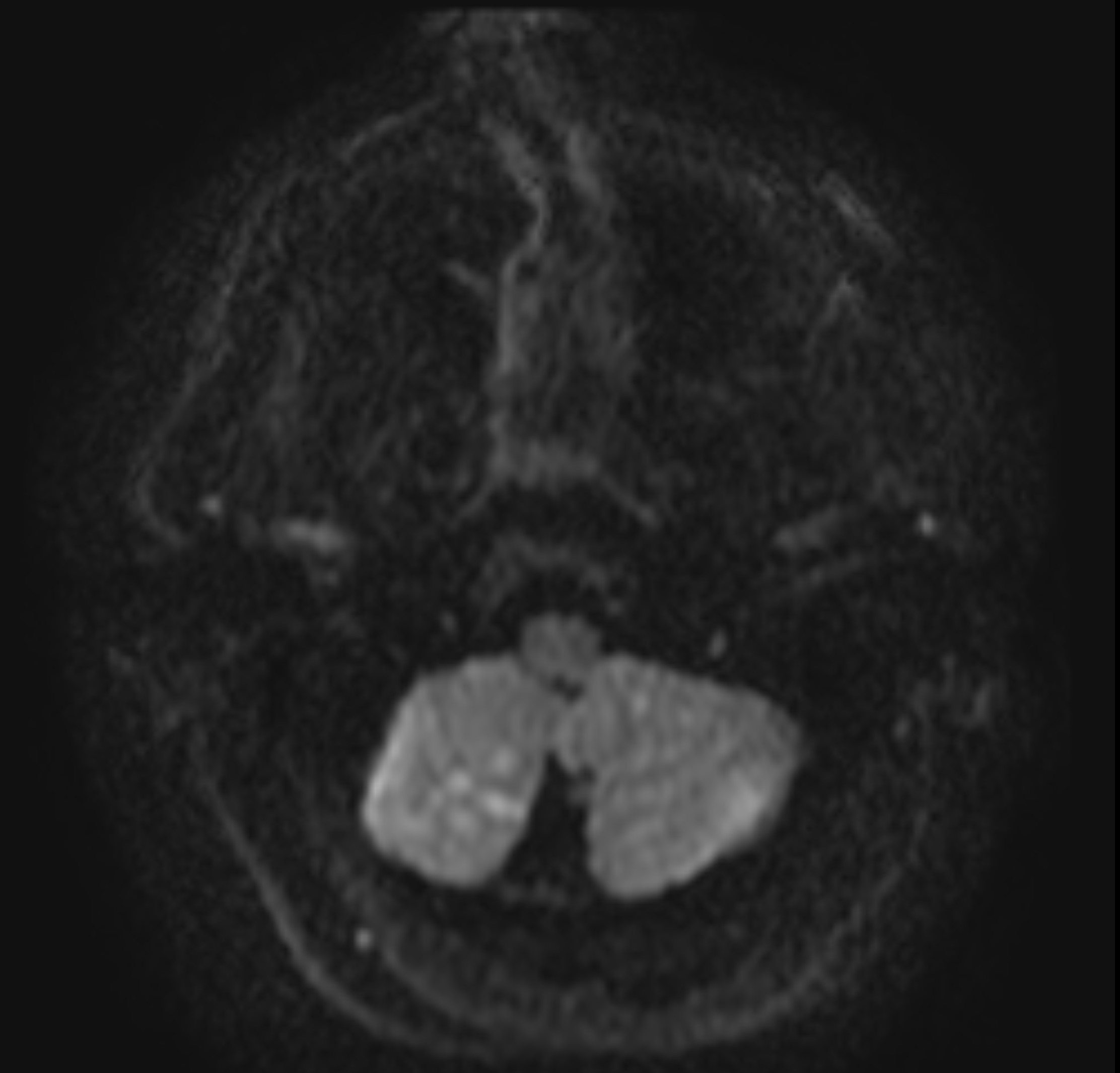
Patients that are treated with embolectomy (and some that are not) receive a follow up MRI to evaluate for infarct burden.
CASE ARCHIVE
Use the following login information to access the case archives: USERNAME: user, PASSWORD: password.
Click here to open up a case archive of basilar thrombus CTA cases
Page Updated: 10.27.22