Page Contents
OVERVIEW
This page is dedicated to covering a very important call case: acute uncomplicated appendicitis. This page will specifically cover this diagnosis in the setting of making the finding on abdomen/pelvis CT imaging.
Many of the cases presented here will be CT scans of the abdomen/pelvis with contrast however certain cases may present non-contrast imaging (which can have overlapping findings).
WHAT IS IT EXACTLY?
Appendicitis refers to inflammation of the appendix. In many cases this is thought to be related to an underlying infectious process, however other inflammatory/reactive processes can be possible as well.
It is important to realize that appendicitis can have a few distinct subcategories with specific imaging characteristics (and with implications on treatment. This page will focus specifically on UNCOMPLICATED appendicitis, however there are separate pages for perforated appendicitis and appendicitis with abscess (both of which are common complications).
WHY IS IT AN IMPORTANT CALL CASE?
Appendicitis is typically regarded as a surgical urgency/emergency as patients can get quite ill (and possibly septic) if it is left untreated too long. While the management of appendicitis has become slightly more nuanced over the years, it is not a self limited condition and requires intervention.
Specifically in the case of acute uncomplicated appendicitis, timely diagnosis and intervention can prevent the development of complications (such as perforation and/or abscess).
WHAT CLINICAL CONTEXT HELPS RAISE SUSPICION FOR THIS DIAGNOSIS?
Patients who present with clinical signs and symptoms of infection (in the setting of abdominal pain) are commonly the demographic that may have appendicitis. Couple clinical details to keep in mind:
- Chief complaint: abdominal pain (may be in the right lower quadrant however not always).
- Relevant medical history: the nature of the abdominal pain may be useful to understand (typically at some point patients will have lower quadrant abdominal pain but this may change location and become more generalized).
- Physical exam: some patients may have rebound tenderness/peritonitis.
- Unstable vitals: while not a requirement, some patients may present with vital signs (tachycardia, hypotension) which may reflect a sepsis type physiology.
- Elevated white count: given the inflammatory process most patients with appendicitis should have a white count (however exceptions may occur).
WHAT IS THE KEY TO MAKING THIS DIAGNOSIS ON CALL?
There are a few imaging features to keep in mind when making this diagnosis. It is important to realize that this is an inflammatory condition, which is reflected in the types of imaging findings we would expect to see. The below video playlist summarizes these findings and applies them to various cases from the associated case archive.
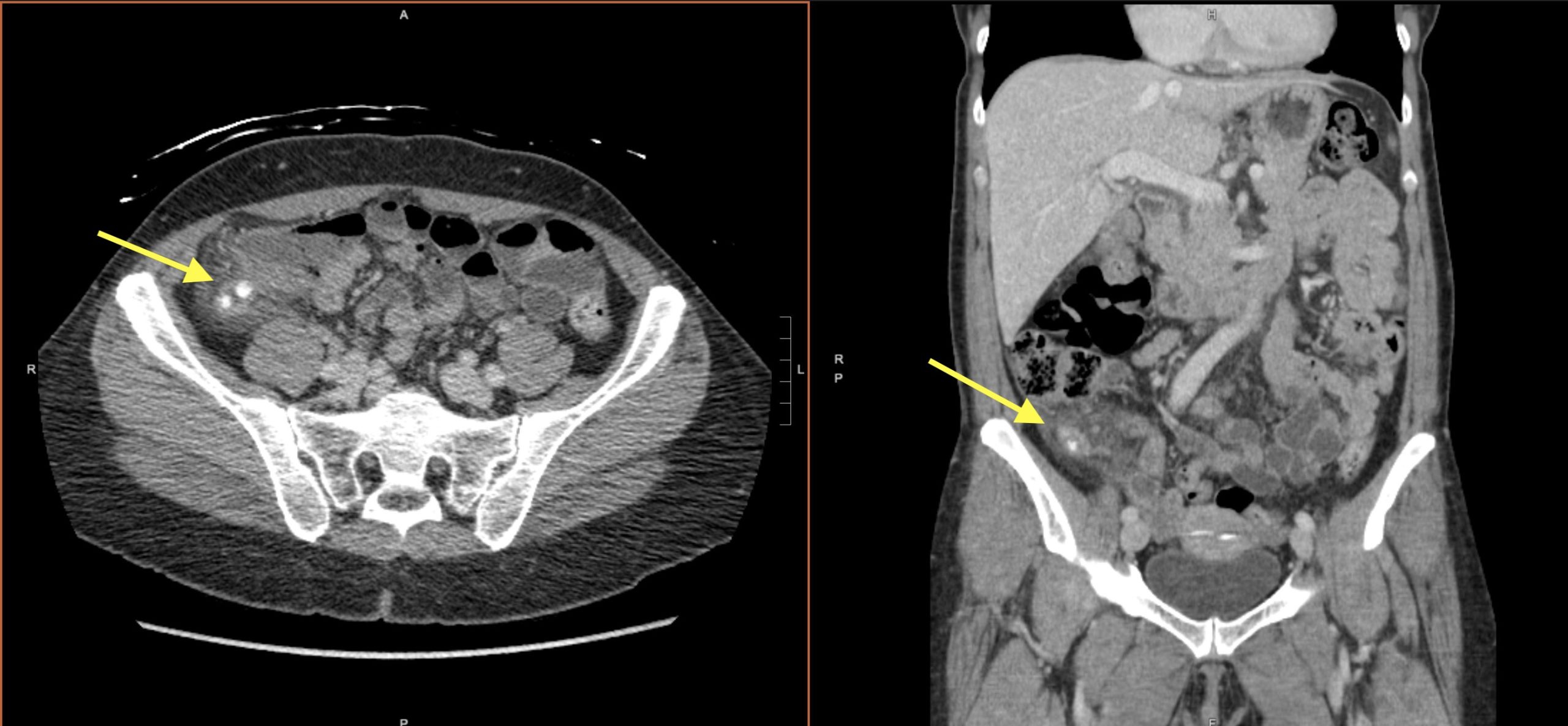
FIRST Find the Terminal Ileum/Ileocecal valve:
While this may appear simple, it is important to make sure that you first identify the appendix. This is to make sure you are not confusing inflammation of another structure as appendicitis (such as the terminal ileum, which has different implications/treatment strategies.
The best way to do this is to first make sure you locate the terminal ileum and the ileocecal valve to understand where the small bowel connects to the cecum.

The ileocecal valve is typically fatty in composition and has a characteristic appearance. Make sure to find this landmark on every case if possible to understand where the ileum connects to the cecum and help locate the appendix. Keep in mind the valve sometimes is not as obvious to see on axial slices, and that you can sometimes see it more easily on coronal/sagittal reformats.
SECOND Find the Appendix:
Once the terminal ileum/ileocecal valve has been correctly identified, the next step is to identify the appendix. This will be a tubular structure that arises from the cecum (near the terminal ileum insertion) and is blind ending.
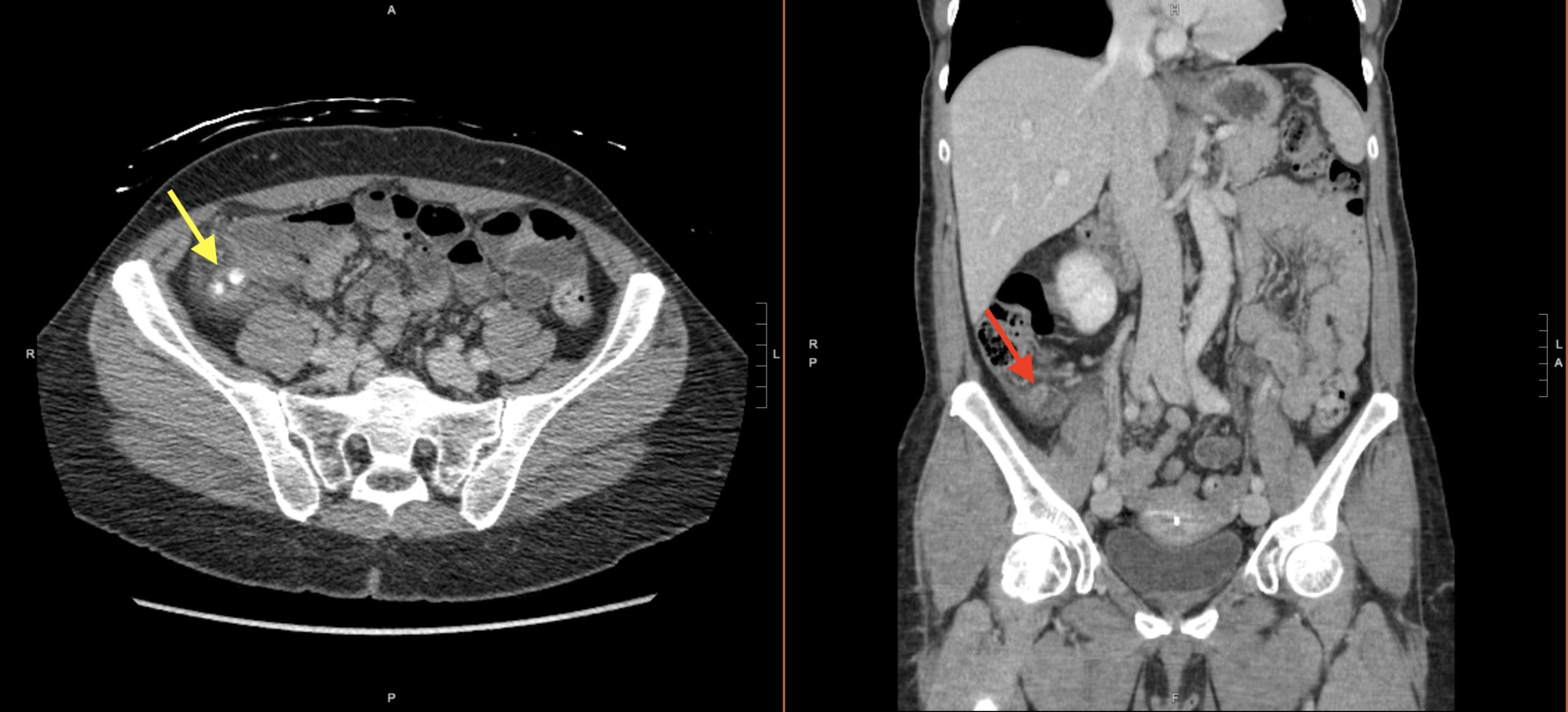
Keep in mind it may take a few scrolls to find the appendix as it can point in most any direction (i.e. retrocecal, up towards the liver, medially, etc). In same cases if its very hard to find…consider investigating if the patient has had an appendectomy!
THIRD Characterize the Appendix:
Now that the appendix has been properly identified, it is time to characterize its features to see if there is suspicion for appendicitis.
Classic features of appendicitis are:
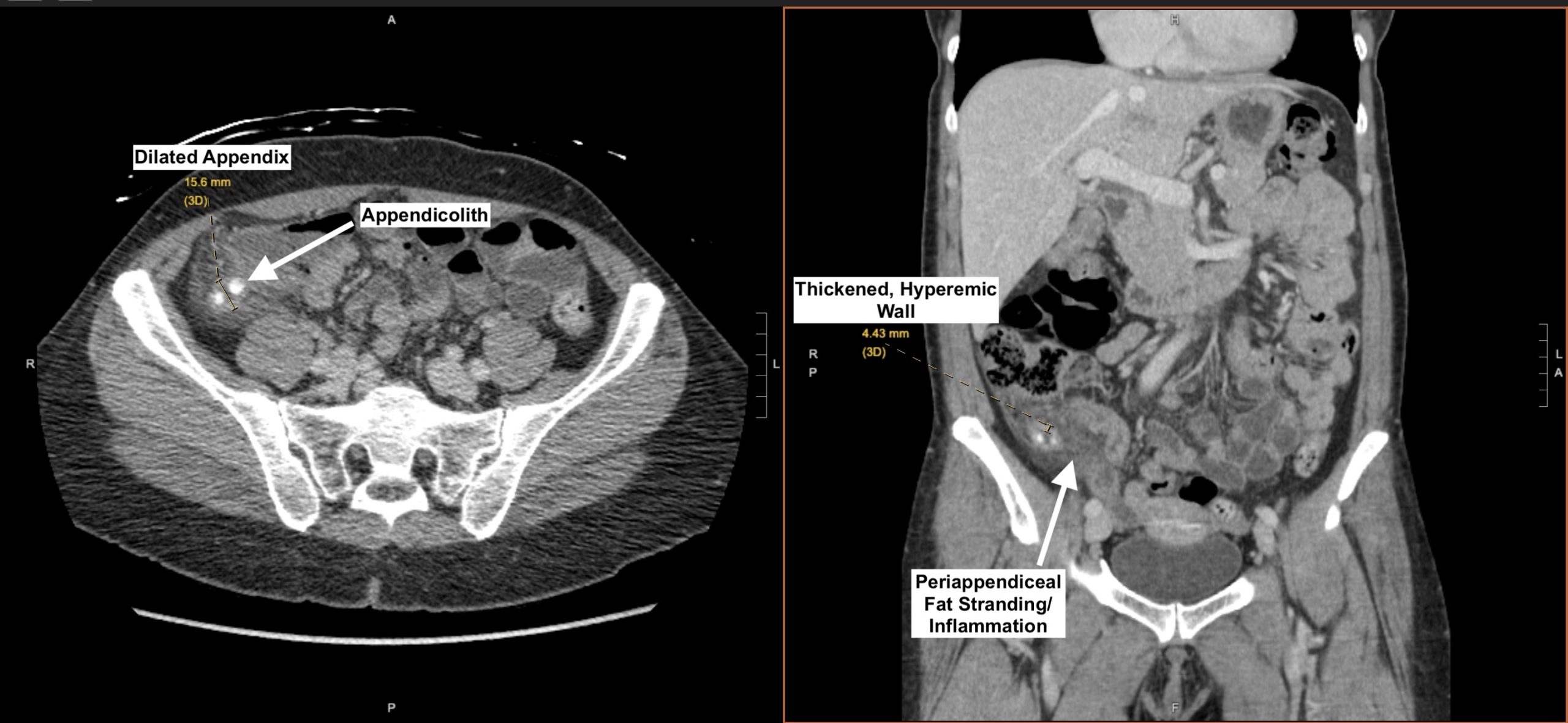
- Periappendiceal inflammation: this may actually be the first finding that is noticed. Periappendiceal fat stranding is often present.
- Dilated appendix diameter: classically appendicitis is thought to result in a dilated appendix diameter of over 6 mm. A normal appendix may measure over 6 mm, however it’s important to always consider if it is possible the a patient has early appendicitis if the appendix is dilated.
- Hyperemic/thickened wall: classically an appendix wall thickness of more than 3 mm raises suspicion for appendicitis (especially in the setting of a hyperenhancing wall).
- Presence of appendicoliths: these calcified deposits within the appendix are characteristic of appendicitis (they also help identify the appendix itself as they are “eye-catching”).
Not every case may have every finding, but the above raise the suspicion for this diagnosis.
FINALLY Look for Complications:
While this page only covers acute uncomplicated appendicitis, it is good to get into the habit of looking for complications as part of your search pattern. Refer to these pages on perforated appendicitis and appendicitis with abscess (both of which are common complications) to learn more.
WHAT HAPPENS NEXT AFTER THE DIAGNOSIS IS MADE?
While treatment pathways ar evolving, typically in the case of acute appendicitis, the patient is taken to the operating room for an appendectomy. This diagnosis has a very clear surgical implication when it is invoked.
CASE ARCHIVE
Use the following login information to access the case archives: USERNAME: user, PASSWORD: password.
Click here to open up a case archive of acute uncomplicated appendicitis seen on CT.
Page Updated: 02.15.23